Final ID: MP2539
In-Hospital, 1-Year and 5-Year Clinical Outcomes of Patients With Severe Aortic Stenosis Treated With Transcatheter Aortic Valve Replacement and Sodium-Glucose Cotransporter 2 Inhibitors
Abstract Body (Do not enter title and authors here): Background: Recent studies have demonstrated that sodium-glucose cotransporter 2 inhibitors (SGLT2i) may reduce procedure-related acute kidney injury (AKI), heart failure readmission and late mortality in patients undergoing transcatheter aortic valve replacement (TAVR).
Hypothesis: We sought to investigate the frequency of use and clinical impact on in-hospital and late TAVR outcomes of SGLT2i in a real-world setting in a high volume TAVR center.
Methods: From a total cohort of 3,333 TAVR procedures performed since 2015, we compared in-hospital, 1-year and 5-year clinical outcomes in 241 patients treated with SGLT2i versus 3,092 without SGLT2i use. Patients received SGLT2i (empagliflozin n=181, dapagliflozin propanediol n=54, or canagliflozin n=6) prior to and following TAVR for treatment of heart failure with diabetes, renal insufficiency and/or left ventricular systolic dysfunction. Dialysis patients and valve-in-valve TAVR procedures were excluded. Propensity-matching was used to adjust for co-variates. AKI was defined by VARC-2 criteria.
Results: Propensity-matched SGLT2i (n=225) and No SGLT2i (n=1,949) cohorts did not differ with respect to baseline characteristics including age (80.0±6.6 vs. 80.9±8.5 years, p=0.061), sex, creatinine, hemoglobin, NYHA class, pre-TAVR echo and cardiac catheterization findings, and STS score (8.9±7.2% vs. 8.0±6.5%, p=0.063). Both groups had similar use of general/conscious sedation anesthesia, femoral/carotid access, balloon-expandable/self-expanding valve type, fluoroscopy time and contrast load (80.0±42.2 vs 84.0±40.3 ml, p=0.248).
SGLT2i versus No SGLT2i patients had similar in-hospital mortality (0.0 vs 0.4%, p=0.0338), ischemic strokes (0.9 vs 1.3%, p=0.575), major vascular complications (2.2 vs 2.5%, p=0.790), and composite bleeding (2.2 vs 2.9%, p=0.576), although SGLT2i patients had a lower incidence of AKI (2.2 vs 6.0%, p=0.020).
At 1-year, the SGLT2i group had lower all-cause mortality (3.2 vs 6.6%, p=0.046) but similar hospital readmission rates (19.1 vs 21.7%, p=0.379) and quality of life KCCQ12 scores (81.7±19.0 vs 81.7±19.1, p=0.071).
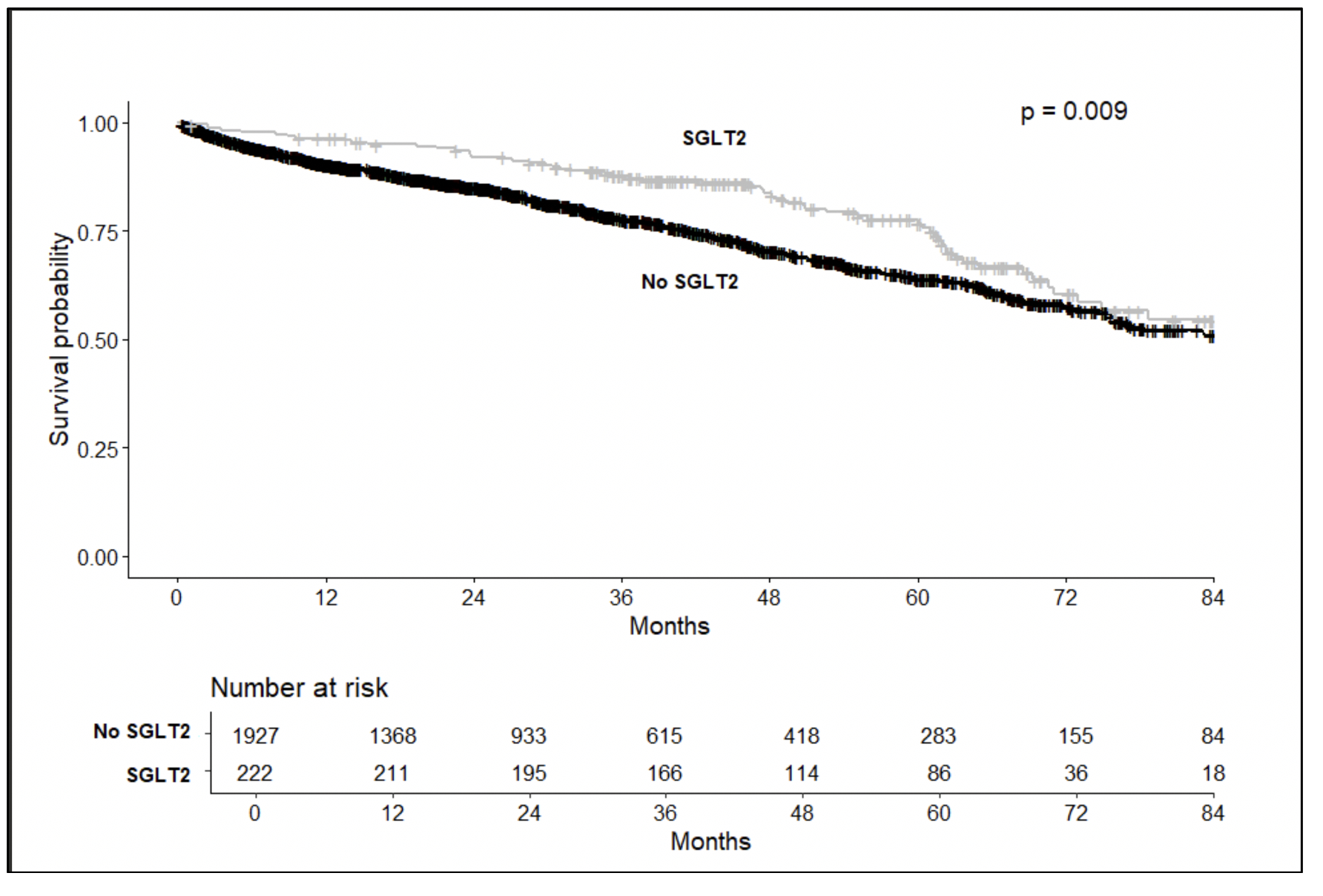
At a mean follow-up of 65.9 (64.2-67.5) months, Kaplan-Meier survival analysis demonstrated lower all-cause mortality in the SGLT2i cohort (p=0.009) (figure).
Conclusion: In this single center study, SGLT2i use was infrequent in patients undergoing TAVR, and was associated with decreased procedural AKI as well as decreased all-cause mortality at 1 and 5-year follow-up.
Hypothesis: We sought to investigate the frequency of use and clinical impact on in-hospital and late TAVR outcomes of SGLT2i in a real-world setting in a high volume TAVR center.
Methods: From a total cohort of 3,333 TAVR procedures performed since 2015, we compared in-hospital, 1-year and 5-year clinical outcomes in 241 patients treated with SGLT2i versus 3,092 without SGLT2i use. Patients received SGLT2i (empagliflozin n=181, dapagliflozin propanediol n=54, or canagliflozin n=6) prior to and following TAVR for treatment of heart failure with diabetes, renal insufficiency and/or left ventricular systolic dysfunction. Dialysis patients and valve-in-valve TAVR procedures were excluded. Propensity-matching was used to adjust for co-variates. AKI was defined by VARC-2 criteria.
Results: Propensity-matched SGLT2i (n=225) and No SGLT2i (n=1,949) cohorts did not differ with respect to baseline characteristics including age (80.0±6.6 vs. 80.9±8.5 years, p=0.061), sex, creatinine, hemoglobin, NYHA class, pre-TAVR echo and cardiac catheterization findings, and STS score (8.9±7.2% vs. 8.0±6.5%, p=0.063). Both groups had similar use of general/conscious sedation anesthesia, femoral/carotid access, balloon-expandable/self-expanding valve type, fluoroscopy time and contrast load (80.0±42.2 vs 84.0±40.3 ml, p=0.248).
SGLT2i versus No SGLT2i patients had similar in-hospital mortality (0.0 vs 0.4%, p=0.0338), ischemic strokes (0.9 vs 1.3%, p=0.575), major vascular complications (2.2 vs 2.5%, p=0.790), and composite bleeding (2.2 vs 2.9%, p=0.576), although SGLT2i patients had a lower incidence of AKI (2.2 vs 6.0%, p=0.020).
At 1-year, the SGLT2i group had lower all-cause mortality (3.2 vs 6.6%, p=0.046) but similar hospital readmission rates (19.1 vs 21.7%, p=0.379) and quality of life KCCQ12 scores (81.7±19.0 vs 81.7±19.1, p=0.071).
At a mean follow-up of 65.9 (64.2-67.5) months, Kaplan-Meier survival analysis demonstrated lower all-cause mortality in the SGLT2i cohort (p=0.009) (figure).
Conclusion: In this single center study, SGLT2i use was infrequent in patients undergoing TAVR, and was associated with decreased procedural AKI as well as decreased all-cause mortality at 1 and 5-year follow-up.
More abstracts on this topic:
Alleviating Aortic Valve Calcification By Blocking TNFα Receptors
Thent Zar Chi, Butcher Jonathan, Zhou Bin
Adverse Events Associated with Early vs. Late SGLT2i Initiation After Heart Failure Hospitalization: A Target Trial Emulation StudyMoon Jungyeon, Naimark David, Stukel Therese, Tu Karen, Ko Dennis, Jackevicius Cynthia, Godoy Lucas, Austin Peter, Chong Alice, Fang Jiming, Odutayo Ayodele, Udell Jacob, Atzema Clare, Booth Gillian