Final ID: MP462
Association of METS-IR and Subclinical Myocardial Injury with Cardiovascular Mortality in U.S. Adults
Abstract Body (Do not enter title and authors here): Background: The Metabolic Score for Insulin Resistance (METS-IR), a non-insulin-based surrogate for insulin resistance (IR), and subclinical myocardial injury (SCMI), defined by abnormal electrocardiogram (ECG) findings, are each associated with cardiovascular (CV) risk. However, their combined impact on CV mortality remains understudied.
Objective: To investigate the association of METS-IR with SCMI, and to assess the individual and combined associations of SCMI and IR with CV mortality.
Methods: We analyzed data from the Third National Health and Nutrition Examination Survey (NHANES III), including participants without known cardiovascular disease. METS-IR was calculated using fasting glucose, triglycerides, high-density lipoprotein cholesterol, and body mass index. High insulin resistance was defined as METS-IR ≥75th percentile. Subclinical myocardial injury was defined by a cardiac infarction injury score (CIIS) of ≥10 on ECG. Participants were grouped by presence or absence of both conditions. Logistic regression was used to evaluate the association of METS-IR with subclinical myocardial injury. Cox proportional hazards models assessed cardiovascular mortality risk across groups, using participants without either condition as the reference.
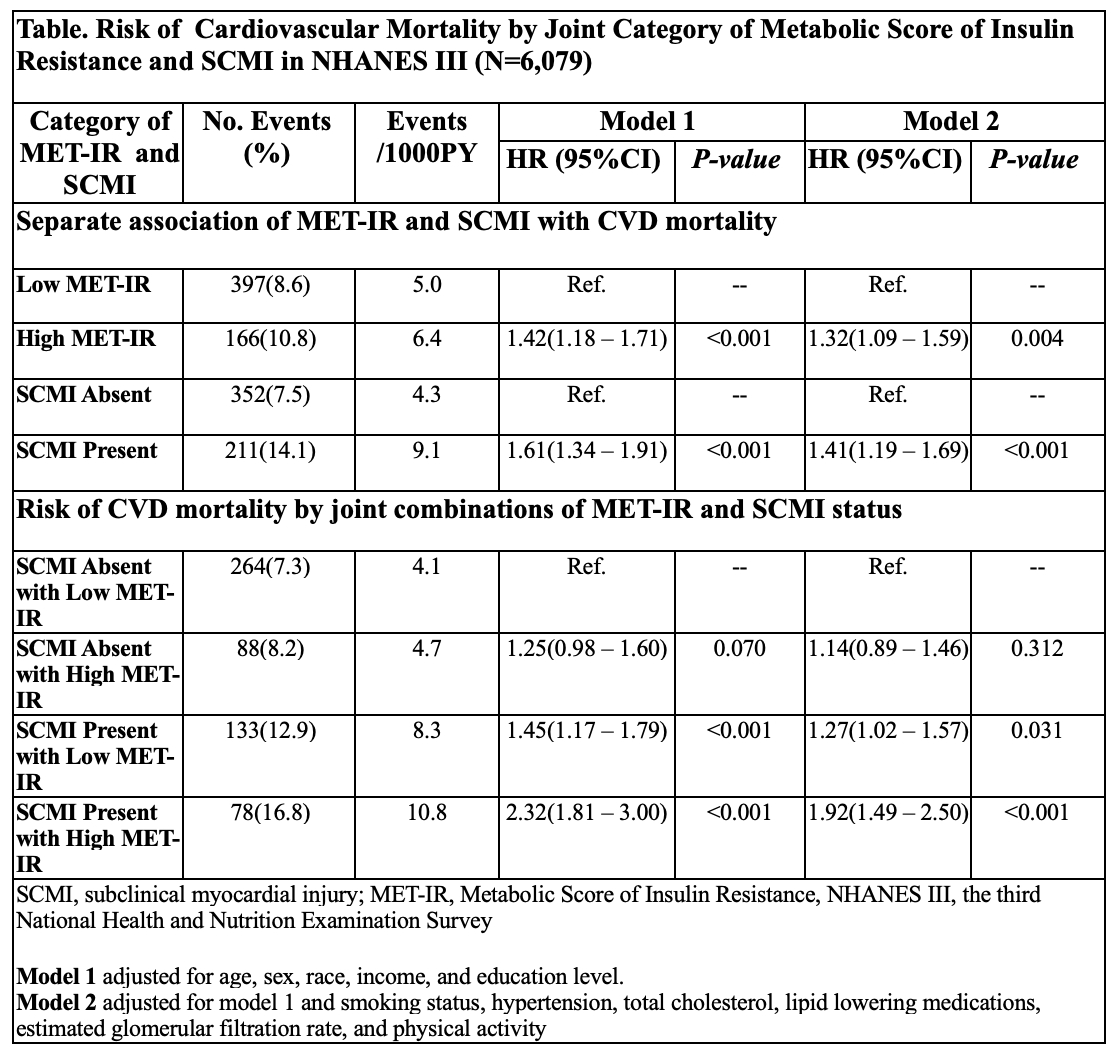
Results: Among 6,079 participants (mean age 55.8 years; 52.4% women), 10.8% had high METS-IR and 14.1% had SCMI. Each standard deviation increase in METS-IR was associated with greater odds of SCMI (OR: 1.20, 95% CI: 1.13–1.28, p<0.001). Over a median follow-up of 18.8 years, 563 CV deaths occurred (9.1%). The presence of either SCMI or high IR was linked to higher CV mortality, with the highest incidence observed in participants with both conditions (16.8% vs. 7.3% for neither). SCMI and high IR were each independently associated with increased CV mortality risk (HR for SCMI: 1.41, 95% CI: 1.19–1.69; HR for high IR: 1.32, 95% CI: 1.09–1.59). Participants with both SCMI and high IR had the highest risk of CV mortality (HR: 1.92, 95% CI: 1.49–2.50). The interaction between CIIS and METS-IR to CV mortality was not statistically significant (p=0.54).
Conclusion: In this nationally representative cohort, METS-IR was positively associated with SCMI. Both SCMI and IR were independently associated with higher CV mortality, and co-occurrence of both identified a subgroup at especially high risk. These findings support the combined use of ECG findings and metabolic risk markers for cardiovascular risk stratification.
Objective: To investigate the association of METS-IR with SCMI, and to assess the individual and combined associations of SCMI and IR with CV mortality.
Methods: We analyzed data from the Third National Health and Nutrition Examination Survey (NHANES III), including participants without known cardiovascular disease. METS-IR was calculated using fasting glucose, triglycerides, high-density lipoprotein cholesterol, and body mass index. High insulin resistance was defined as METS-IR ≥75th percentile. Subclinical myocardial injury was defined by a cardiac infarction injury score (CIIS) of ≥10 on ECG. Participants were grouped by presence or absence of both conditions. Logistic regression was used to evaluate the association of METS-IR with subclinical myocardial injury. Cox proportional hazards models assessed cardiovascular mortality risk across groups, using participants without either condition as the reference.
Results: Among 6,079 participants (mean age 55.8 years; 52.4% women), 10.8% had high METS-IR and 14.1% had SCMI. Each standard deviation increase in METS-IR was associated with greater odds of SCMI (OR: 1.20, 95% CI: 1.13–1.28, p<0.001). Over a median follow-up of 18.8 years, 563 CV deaths occurred (9.1%). The presence of either SCMI or high IR was linked to higher CV mortality, with the highest incidence observed in participants with both conditions (16.8% vs. 7.3% for neither). SCMI and high IR were each independently associated with increased CV mortality risk (HR for SCMI: 1.41, 95% CI: 1.19–1.69; HR for high IR: 1.32, 95% CI: 1.09–1.59). Participants with both SCMI and high IR had the highest risk of CV mortality (HR: 1.92, 95% CI: 1.49–2.50). The interaction between CIIS and METS-IR to CV mortality was not statistically significant (p=0.54).
Conclusion: In this nationally representative cohort, METS-IR was positively associated with SCMI. Both SCMI and IR were independently associated with higher CV mortality, and co-occurrence of both identified a subgroup at especially high risk. These findings support the combined use of ECG findings and metabolic risk markers for cardiovascular risk stratification.
More abstracts on this topic:
Albuminuria Drives Type 2 Diabetes-Related Atrial Fibrillation: an ACCORD substudy
Siqueira Amanda, Everett Brendan
Ceramide Mediated Inhibition of Regulatory T Cell Function Impairs Metabolic HomeostasisThakkar Himani, Summers Scott, Teghanemt Athmane, Issuree Priya, Hale Scott, Chaurasia Bhagirath, Ksiazek Alec, Chandranvanshi Bhawna, Anand Ajay, Vincent Vinnyfred, Naderi Jamal, Johnson Amanda, Tran Aaron, Maschek J. Alan