Final ID: Mo3145
Relationship between Triglyceride-Glucose Index, Subclinical Myocardial Injury, and Cardiovascular Mortality in NHANES III
Abstract Body (Do not enter title and authors here): Background: Subclinical myocardial injury (SCMI) and the triglyceride-glucose index (TyG), a marker for insulin resistance, are each linked to cardiovascular (CV) mortality. The impact of both SCMI and TyG on CV mortality is unclear.
Objective: To investigate the relationship between TyG, SCMI, and CV mortality.
Methods: This study utilized data from the third National Health and Nutrition Examination Survey (NHANES-III) including participants without cardiovascular disease (CVD). Baseline TyG was calculated as ln(fasting triglyceride level [mg/dL] × fasting plasma glucose [mg/dL]/2). High TyG was defined as ≥75th percentile, and low TyG as <75th percentile. SCMI was identified by an electrocardiogram (ECG) cardiac infarction injury score ≥10. CV mortality data was sourced from the National Death Index. Associations of TyG with SCMI were analyzed using multivariate logistic regression, and Cox proportional hazards models assessed the individual and combined associations of TyG and SCMI with CV mortality.
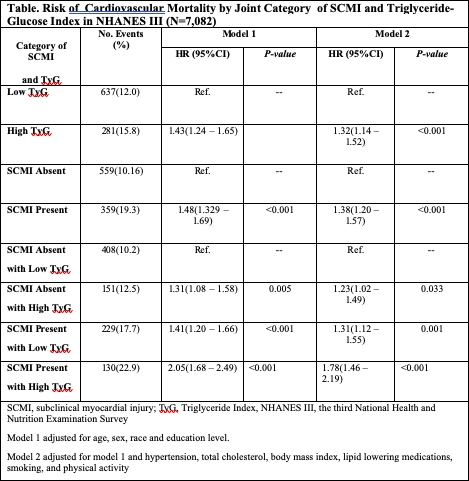
Results: Of 7,082 participants (mean age 59.3±13.4 years; 52.8% women; 49.4% White), 1,775 (25.1%) had high TyG and 1,860 (26.3%) had SCMI. High TyG was associated with higher odds of SCMI (odds ratio (OR): 1.38, 95% CI: 1.21–1.57, p<0.0001) and each unit increase in TyG corresponded to increased SCMI risk (OR: 1.27, 95% CI: 1.16–1.39, p<0.0001). High TyG and SCMI were linked to 32% and 38% higher CV mortality risk, respectively. Participants with both high TyG and SCMI had a significantly higher risk of CV mortality (Hazard ratio (HR): 1.78, 95% CI: 1.46–2.19) compared to those with low TyG and no SCMI (see Table). The interaction between SCMI and TyG in the fully adjusted Cox Model 2 (see Table) was not statistically significant (p=0.45).
Conclusions: In NHANES III adults without CVD, TyG was associated with SCMI. Both high TyG and SCMI independently increased CV mortality risk, with the greatest risk observed in individuals with both conditions. Further research is needed to evaluate the effectiveness of these markers in CVD risk assessment and explore interventions to mitigate this risk.
Objective: To investigate the relationship between TyG, SCMI, and CV mortality.
Methods: This study utilized data from the third National Health and Nutrition Examination Survey (NHANES-III) including participants without cardiovascular disease (CVD). Baseline TyG was calculated as ln(fasting triglyceride level [mg/dL] × fasting plasma glucose [mg/dL]/2). High TyG was defined as ≥75th percentile, and low TyG as <75th percentile. SCMI was identified by an electrocardiogram (ECG) cardiac infarction injury score ≥10. CV mortality data was sourced from the National Death Index. Associations of TyG with SCMI were analyzed using multivariate logistic regression, and Cox proportional hazards models assessed the individual and combined associations of TyG and SCMI with CV mortality.
Results: Of 7,082 participants (mean age 59.3±13.4 years; 52.8% women; 49.4% White), 1,775 (25.1%) had high TyG and 1,860 (26.3%) had SCMI. High TyG was associated with higher odds of SCMI (odds ratio (OR): 1.38, 95% CI: 1.21–1.57, p<0.0001) and each unit increase in TyG corresponded to increased SCMI risk (OR: 1.27, 95% CI: 1.16–1.39, p<0.0001). High TyG and SCMI were linked to 32% and 38% higher CV mortality risk, respectively. Participants with both high TyG and SCMI had a significantly higher risk of CV mortality (Hazard ratio (HR): 1.78, 95% CI: 1.46–2.19) compared to those with low TyG and no SCMI (see Table). The interaction between SCMI and TyG in the fully adjusted Cox Model 2 (see Table) was not statistically significant (p=0.45).
Conclusions: In NHANES III adults without CVD, TyG was associated with SCMI. Both high TyG and SCMI independently increased CV mortality risk, with the greatest risk observed in individuals with both conditions. Further research is needed to evaluate the effectiveness of these markers in CVD risk assessment and explore interventions to mitigate this risk.
More abstracts on this topic:
Blood Pressure Measures are Not Associated with Early Metabolic Imbalance: The U.S. National Health and Nutrition Examination Survey
Mendiola Luis, Dwivedi Alok, Cistola David
Activated CD8+HLA-DR+ T Cells as Immune Biomarkers of Metabolic Dysfunction and Cardiovascular Risk in PrediabetesAlrashed Fatema, Alsaeed Halemah, Alturaiki Wael, Akhter Nadeem, Alosaimi Bandar, Almutairi Saeedah, Mubarak Ayman, Al-mulla Fahd, Ahmad Rasheed