Final ID: 4351680
Madly Dangerous: Unmasking the Arrhythmogenic Nature of Valvular Heart Disease
Abstract Body (Do not enter title and authors here): A 36-year-old woman (G2P1) at 8 weeks gestation, with a few days of nonbilious vomiting, presented following an out-of-hospital ventricular fibrillation (VF) cardiac arrest. Return of spontaneous circulation was achieved after multiple defibrillation attempts. Given ongoing sustained ventricular tachycardia (VT), she was intubated and cannulated for extracorporeal membrane oxygenation (ECMO).
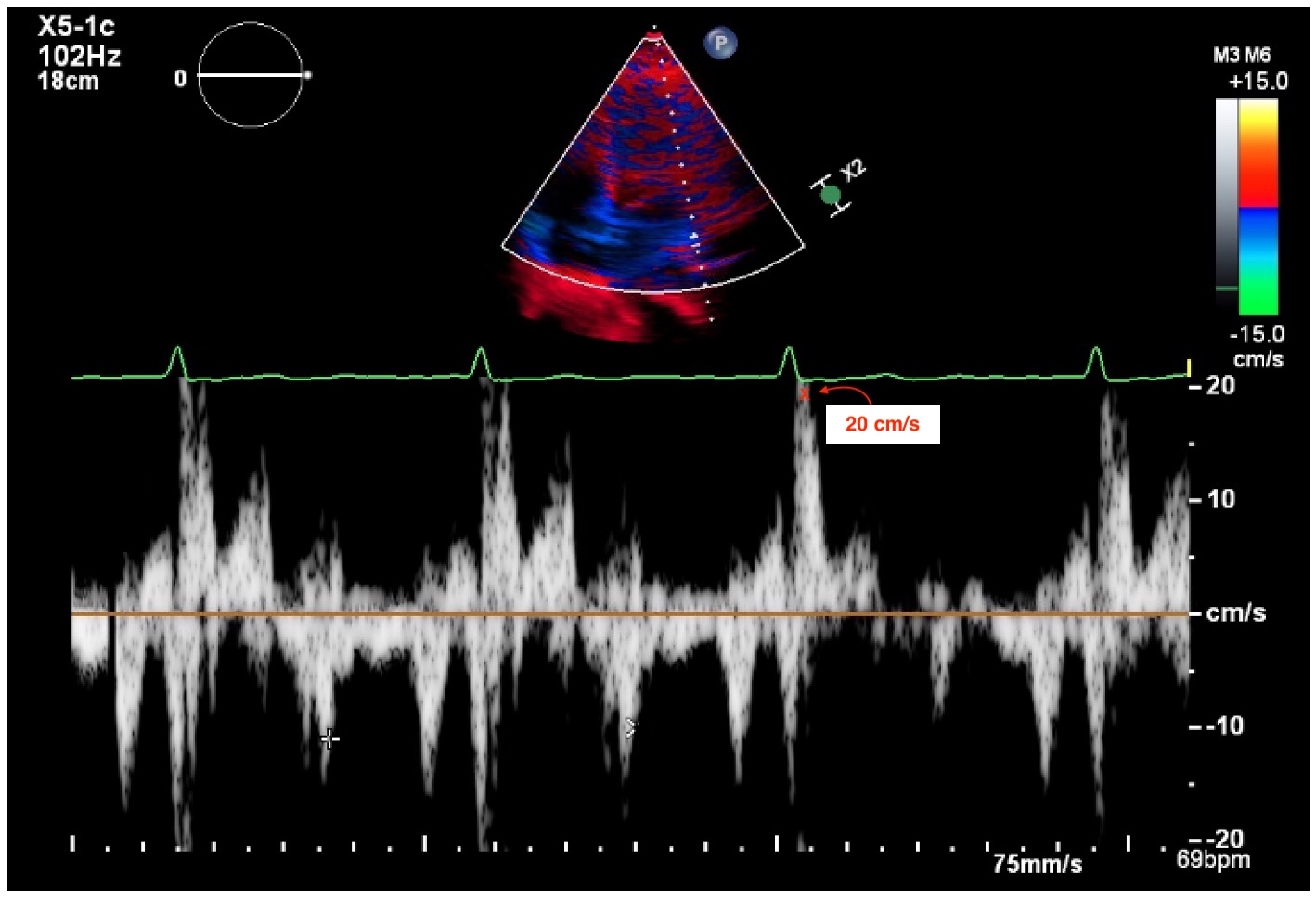
Initial transthoracic echocardiography revealed reduced left ventricular ejection fraction (LVEF) and mitral annular disjunction (MAD), with a peak lateral mid-systolic velocity of 20 cm/s (Figure 1). Left heart catheterization showed normal coronary arteries and a right heart catheterization raised concerns for intravascular volume depletion.
Her hospital course was complicated by abdominal distension and a drop in hemoglobin, raising suspicion for peritoneal bleeding. A CT aortogram confirmed hemoperitoneum, and a transvaginal ultrasound showed no intrauterine pregnancy. She underwent emergent surgical evacuation of a ruptured ectopic pregnancy with right salpingectomy.
Postoperatively, she experienced persistent polymorphic VT and prolonged QTc. Amiodarone was discontinued and she was initiated on lidocaine for VT management. Notably, a Holter monitor four years prior had shown non-sustained monomorphic and polymorphic VT. A cardiac MRI (CMR) at that time demonstrated normal LVEF with evidence of myocardial fibrosis, but the patient deferred treatment and was lost to follow-up.
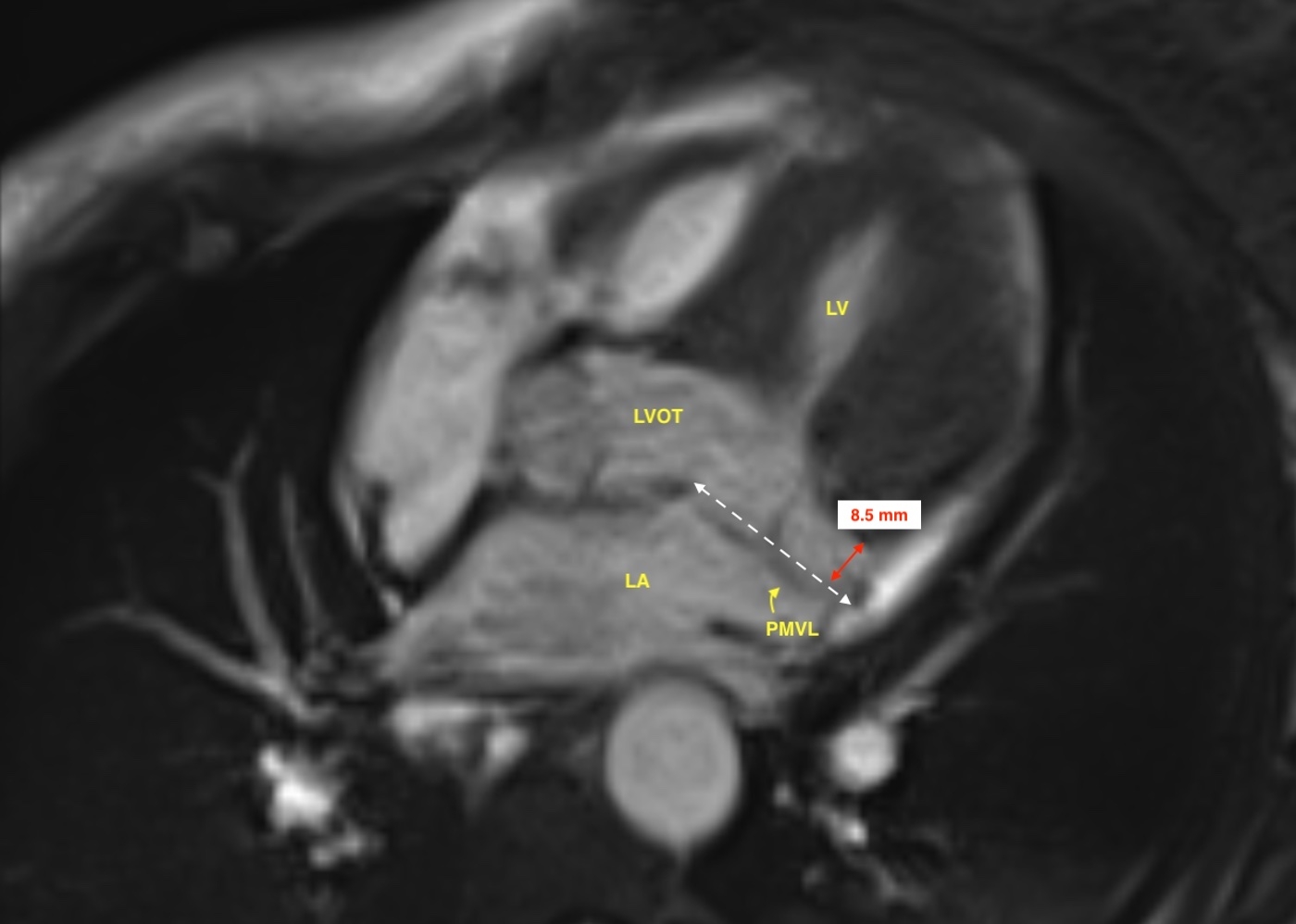
Following stabilization, the patient’s LVEF recovered, and she was successfully decannulated from ECMO. Repeat CMR prior to discharge confirmed bileaflet mitral valve prolapse with MAD measuring 8.5 mm in length (Figure 2). She was transitioned to oral antiarrhythmic therapy and underwent subcutaneous implantable cardioverter-defibrillator (ICD) placement. Outpatient genetic testing was negative.
MAD is a recognized substrate for out-of-hospital cardiac arrest. In this patient, the presence of MAD, along with a catecholamine surge from a ruptured ectopic pregnancy and acute hypokalemia from vomiting, likely created a highly proarrhythmic state. High-risk features in MAD associated with arrhythmic events include bileaflet mitral valve prolapse, myocardial fibrosis on CMR, MAD length equal to or >8.5 mm, and peak lateral mid-systolic velocity >16 cm/s. ICD implantation should be considered in patients with these characteristics, particularly those with sustained ventricular arrhythmias.
Initial transthoracic echocardiography revealed reduced left ventricular ejection fraction (LVEF) and mitral annular disjunction (MAD), with a peak lateral mid-systolic velocity of 20 cm/s (Figure 1). Left heart catheterization showed normal coronary arteries and a right heart catheterization raised concerns for intravascular volume depletion.
Her hospital course was complicated by abdominal distension and a drop in hemoglobin, raising suspicion for peritoneal bleeding. A CT aortogram confirmed hemoperitoneum, and a transvaginal ultrasound showed no intrauterine pregnancy. She underwent emergent surgical evacuation of a ruptured ectopic pregnancy with right salpingectomy.
Postoperatively, she experienced persistent polymorphic VT and prolonged QTc. Amiodarone was discontinued and she was initiated on lidocaine for VT management. Notably, a Holter monitor four years prior had shown non-sustained monomorphic and polymorphic VT. A cardiac MRI (CMR) at that time demonstrated normal LVEF with evidence of myocardial fibrosis, but the patient deferred treatment and was lost to follow-up.
Following stabilization, the patient’s LVEF recovered, and she was successfully decannulated from ECMO. Repeat CMR prior to discharge confirmed bileaflet mitral valve prolapse with MAD measuring 8.5 mm in length (Figure 2). She was transitioned to oral antiarrhythmic therapy and underwent subcutaneous implantable cardioverter-defibrillator (ICD) placement. Outpatient genetic testing was negative.
MAD is a recognized substrate for out-of-hospital cardiac arrest. In this patient, the presence of MAD, along with a catecholamine surge from a ruptured ectopic pregnancy and acute hypokalemia from vomiting, likely created a highly proarrhythmic state. High-risk features in MAD associated with arrhythmic events include bileaflet mitral valve prolapse, myocardial fibrosis on CMR, MAD length equal to or >8.5 mm, and peak lateral mid-systolic velocity >16 cm/s. ICD implantation should be considered in patients with these characteristics, particularly those with sustained ventricular arrhythmias.
More abstracts on this topic:
A Rare Case Of Localized Ventricular Tachycardia Due To Mitral Annular Disjunction And a Subvalvular Aneurysm
O'toole Timothy, Binder Michael, Hama Amin Ali
Divergent Biventricular Mechano-Energetic Responses to VA-ECMO Flow Ramping After Cardiac Arrest: A Preclinical ECPR Swine ModelOwyang Clark, King Andrea, Finkelstein Robert, Berlin David, Martin-flores Manuel, Heerdt Paul, Araos Joaquin, Teran Felipe, Landau Aaron, Suh Caleb, Satalin Joshua, Lopez Daniel, Searles Bruce, Nejatollahi Maryam, Kulthinee Supaporn