Final ID: MDP1516
Analysis of In-Hospital Outcomes of Transcatheter Edge-to-Edge Repair of Mitral Valve in Patients with and without COVID-19: Insights from the National Inpatient Sample Data (2020-2021)
Abstract Body (Do not enter title and authors here): Background:
COVID-19 has introduced new complexities in the management of patients undergoing the transcatheter edge-to-edge repair (TEER) procedure of the mitral valve. This study compares outcomes of mitral valve TEER in patients with and without COVID-19, utilizing data from the National Inpatient Sample (2020-2021).
Methods:
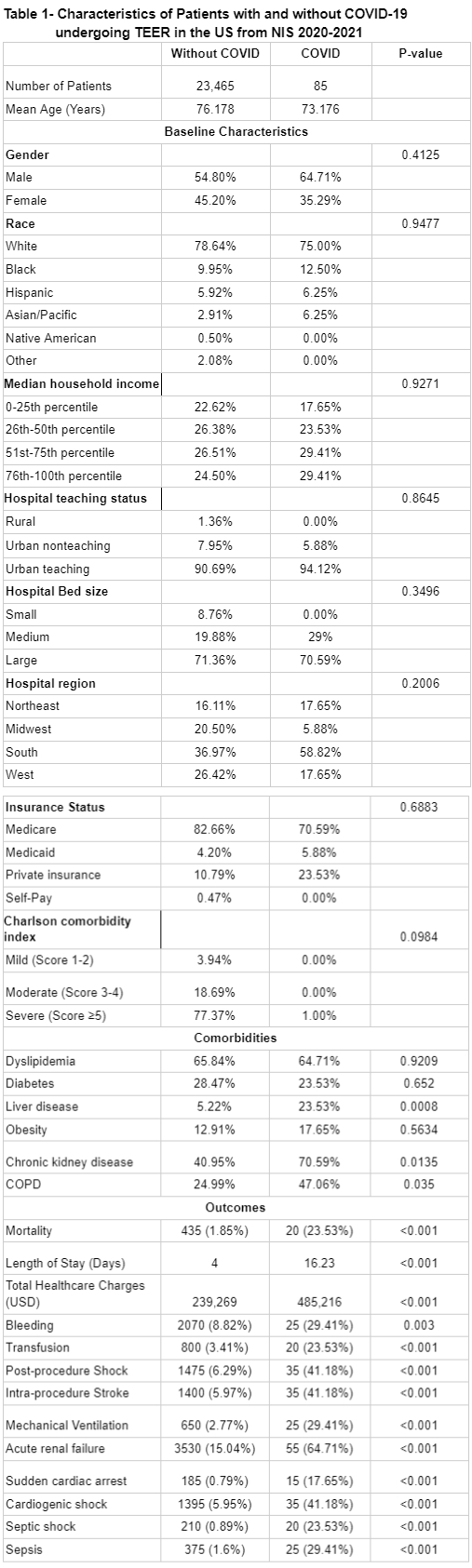
We conducted a retrospective cohort study on 23,465 patients without COVID-19 and 85 patients with COVID-19 undergoing mitral valve TEER. Multivariate logistic regression was employed to compare outcomes, adjusting for potential confounders. Primary outcomes included mortality and major complications, while secondary outcomes encompassed specific procedural complications.
Results:
Patients with COVID-19 were younger (mean age: 73.176 vs. 76.178 years, p-value <0.001) and exhibited differences in gender distribution (male: 64.71% vs. 54.80%, female: 35.29% vs. 45.20%, p=0.4125)
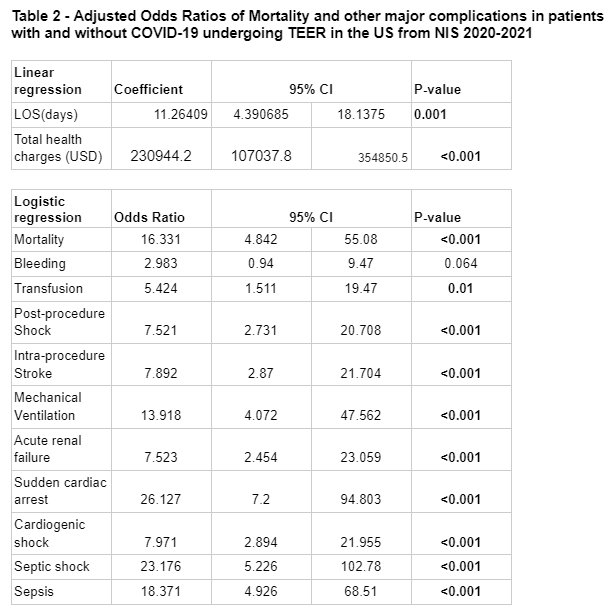
Patients with COVID-19 exhibited a significantly higher prevalence of mortality (OR: 16.331, 95% CI: 4.842-55.08, p<0.001), transfusion (OR: 5.424, 95% CI: 1.511-19.47, p=0.01), post-procedure shock (OR: 7.521, 95% CI: 2.731-20.708, p<0.001), intra-procedure stroke (OR: 7.892, 95% CI: 2.87-21.704, p<0.001), mechanical ventilation (OR: 13.918, 95% CI: 4.072-47.562, p<0.001), acute renal failure (OR: 7.523, 95% CI: 2.454-23.059, p<0.001), sudden cardiac arrest (OR: 26.127, 95% CI: 7.2-94.803, p<0.001), cardiogenic shock (OR: 7.971, 95% CI: 2.894-21.955, p<0.001), septic shock (OR: 23.176, 95% CI: 5.226-102.78, p<0.001), and sepsis (OR: 18.371, 95% CI: 4.926-68.51, p<0.001). The odds of bleeding (OR: 2.983, 95% CI: 0.94-9.47, p=0.064) did not significantly differ between groups.
Patients with COVID-19 had a longer length of stay (LOS) (coefficient: 11.26409 days, p=0.001) and higher total hospitalization cost (coefficient: $230,944.2, 95% CI: $107,037.8-$354,850.5, p<0.001).
Conclusion:
Patients with COVID-19 undergoing mitral valve TEER procedure face elevated risks of mortality, post-procedure shock, stroke, mechanical ventilation, acute renal failure, sudden cardiac arrest, cardiogenic shock, septic shock, and sepsis compared to those without COVID-19. Additionally, they experience longer hospital stays and incur higher total health charges. Clinicians should consider these heightened risks when evaluating the appropriateness of mitral valve TEER in COVID-19 patients. Further research is warranted to explore strategies for risk mitigation in this population.
COVID-19 has introduced new complexities in the management of patients undergoing the transcatheter edge-to-edge repair (TEER) procedure of the mitral valve. This study compares outcomes of mitral valve TEER in patients with and without COVID-19, utilizing data from the National Inpatient Sample (2020-2021).
Methods:
We conducted a retrospective cohort study on 23,465 patients without COVID-19 and 85 patients with COVID-19 undergoing mitral valve TEER. Multivariate logistic regression was employed to compare outcomes, adjusting for potential confounders. Primary outcomes included mortality and major complications, while secondary outcomes encompassed specific procedural complications.
Results:
Patients with COVID-19 were younger (mean age: 73.176 vs. 76.178 years, p-value <0.001) and exhibited differences in gender distribution (male: 64.71% vs. 54.80%, female: 35.29% vs. 45.20%, p=0.4125)
Patients with COVID-19 exhibited a significantly higher prevalence of mortality (OR: 16.331, 95% CI: 4.842-55.08, p<0.001), transfusion (OR: 5.424, 95% CI: 1.511-19.47, p=0.01), post-procedure shock (OR: 7.521, 95% CI: 2.731-20.708, p<0.001), intra-procedure stroke (OR: 7.892, 95% CI: 2.87-21.704, p<0.001), mechanical ventilation (OR: 13.918, 95% CI: 4.072-47.562, p<0.001), acute renal failure (OR: 7.523, 95% CI: 2.454-23.059, p<0.001), sudden cardiac arrest (OR: 26.127, 95% CI: 7.2-94.803, p<0.001), cardiogenic shock (OR: 7.971, 95% CI: 2.894-21.955, p<0.001), septic shock (OR: 23.176, 95% CI: 5.226-102.78, p<0.001), and sepsis (OR: 18.371, 95% CI: 4.926-68.51, p<0.001). The odds of bleeding (OR: 2.983, 95% CI: 0.94-9.47, p=0.064) did not significantly differ between groups.
Patients with COVID-19 had a longer length of stay (LOS) (coefficient: 11.26409 days, p=0.001) and higher total hospitalization cost (coefficient: $230,944.2, 95% CI: $107,037.8-$354,850.5, p<0.001).
Conclusion:
Patients with COVID-19 undergoing mitral valve TEER procedure face elevated risks of mortality, post-procedure shock, stroke, mechanical ventilation, acute renal failure, sudden cardiac arrest, cardiogenic shock, septic shock, and sepsis compared to those without COVID-19. Additionally, they experience longer hospital stays and incur higher total health charges. Clinicians should consider these heightened risks when evaluating the appropriateness of mitral valve TEER in COVID-19 patients. Further research is warranted to explore strategies for risk mitigation in this population.
More abstracts on this topic:
A Rare Case of Purulent Methicillin-Resistant Staphylococcus Aureus Pericarditis Presenting with Septic Shock
Elisarraras Francisco, Roberts Jacob, Hindosh Ziad, Arega Enat, Madnick David, Cruz Daniel, Srivastava Pratyaksh
A Rare Case of Mycotic Pseudoaneurysm in a Pediatric Patient with a History of Disseminated MRSAAmilhamja Anissa, Shaikh Adam, Porisch Mary