Final ID: MP2307
Differential Associations by Sex Between Sleep-Wake Regularity and All-Cause and Cardiovascular Mortality
Abstract Body (Do not enter title and authors here): Introduction
Highly irregular sleep-wake timing is prospectively associated with higher all-cause and cardiovascular (CVD) mortality rates. These relationships are hypothesized to reflect harmful effects of inconsistent patterns of exposures (eg, light-dark), behaviors (eg, sleep-wake), and circadian rhythms (ie, intrinsic time-varying physiology). Sex differences span sleep and circadian physiology, yet sex-specific relationships between sleep regularity and mortality have not been assessed.
Question
Using the Sleep Regularity Index (SRI), a metric that captures circadian disruption through the average probability that participants are in the same sleep-wake state 24 hours apart, this study examined whether associations between the day-to-day regularity of sleep-wake timing and mortality differ by sex.
Methods
The study included UK Biobank participants with week-long accelerometer-derived sleep-wake data. To reduce reverse causality bias, deaths within one year of recordings were excluded. SRI was calculated by sleepreg. All-cause and CVD mortality were ascertained from inpatient hospital records and death registrars. Age-adjusted Cox proportional hazards models estimated adjusted hazards ratios (aHRs) between SRI categories and time to all-cause or CVD mortality without and with SRI × sex interaction term. SRI–sex combinations were compared using estimated marginal means.
Results
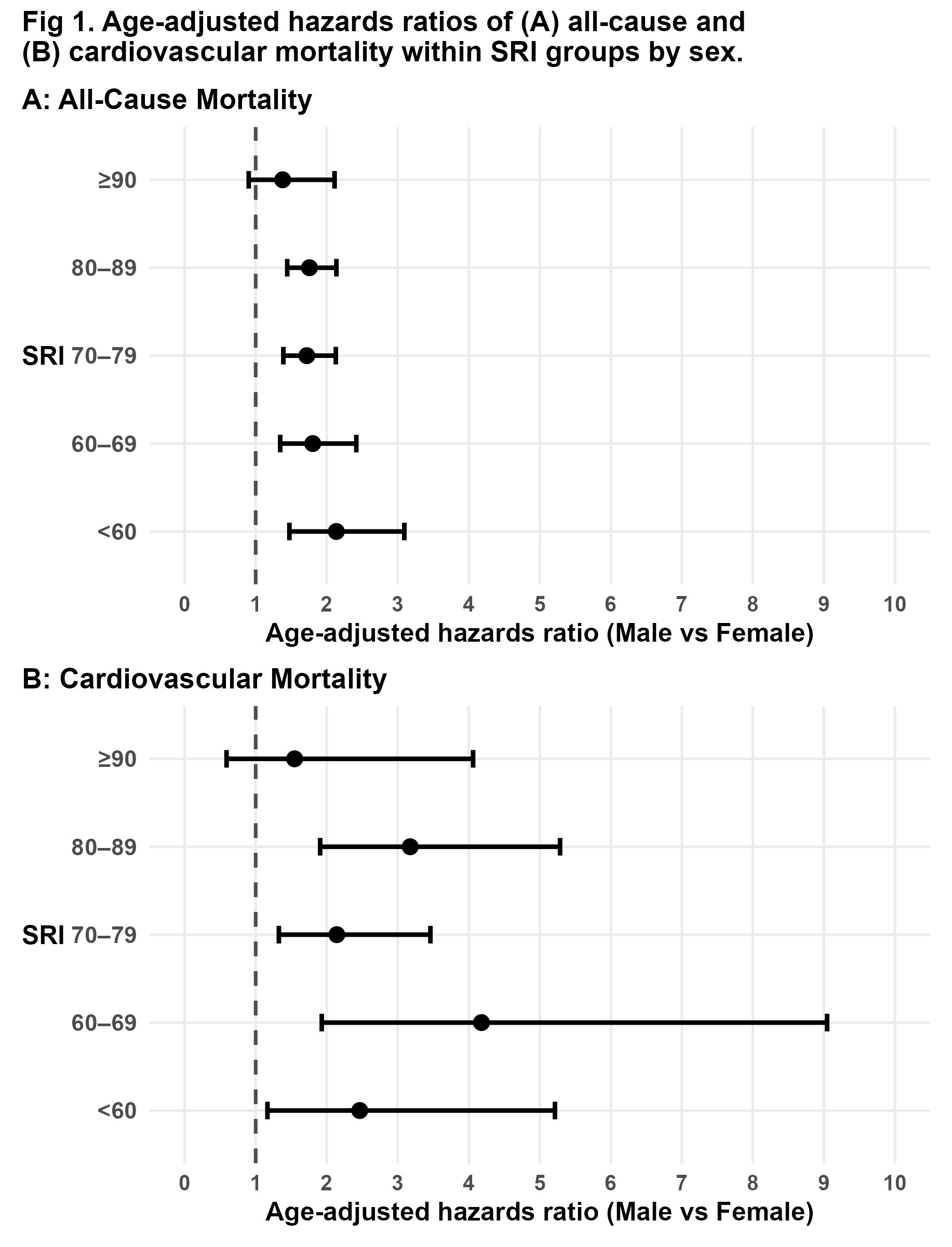
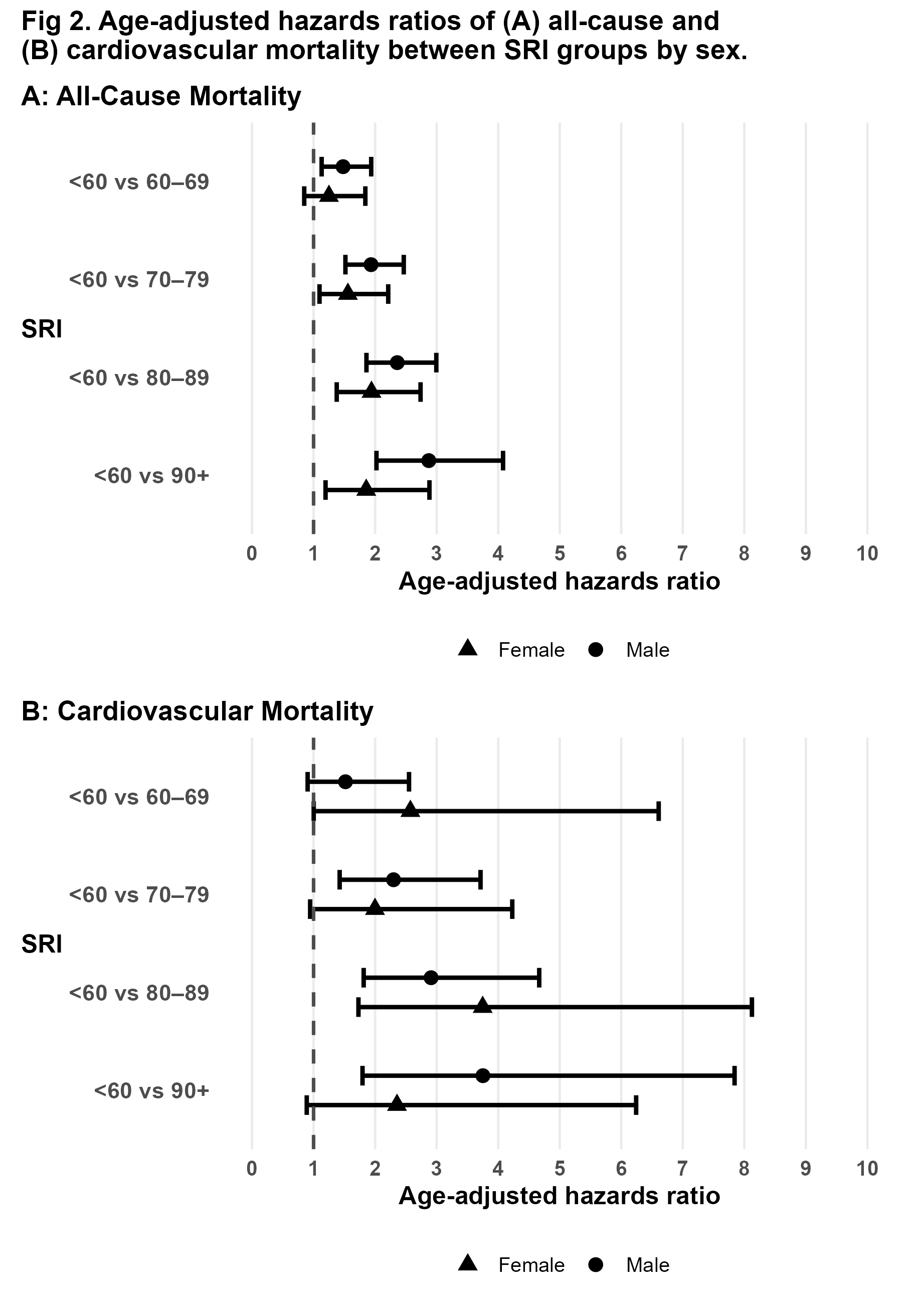
Among 73,647 adults (41,489 [56.3%] female, mean age 62.5±7.8 y) followed for a mean of 7.5±0.9 y, there were 2631 deaths; 20.5% were from primarily CVD causes. Higher age-adjusted mortality rates were observed with the lowest SRI (<60) compared to the highest (≥90) for both all-cause (aHR=2.4; 95% CI=2.0–2.9) and CVD mortality (3.2; 2.1–4.6) (Fig 1). Significant interaction terms were identified for SRI <60 × male (all-cause) and SRI 60–69 × male (CVD). Higher all-cause and CVD mortality rates were associated among males with SRI <60 versus ≥90 (all-cause 2.9; 2.1–4.0; CVD 3.8; 1.9–7.5) and compared to females with SRI <60 (all-cause 2.1; 1.5–3.0; CVD 2.5; 1.2–5.0) (Fig 2). In contrast, neither all-cause nor CVD mortality differed by sex among individuals with SRI ≥90.
Conclusion
Higher mortality rates associated with highly irregular sleep-wake timing are particularly pronounced among males, especially for CVD mortality. The absence of sex differences among those with high sleep regularity suggests that consistent sleep-wake patterns may attenuate heightened male mortality rates.
Highly irregular sleep-wake timing is prospectively associated with higher all-cause and cardiovascular (CVD) mortality rates. These relationships are hypothesized to reflect harmful effects of inconsistent patterns of exposures (eg, light-dark), behaviors (eg, sleep-wake), and circadian rhythms (ie, intrinsic time-varying physiology). Sex differences span sleep and circadian physiology, yet sex-specific relationships between sleep regularity and mortality have not been assessed.
Question
Using the Sleep Regularity Index (SRI), a metric that captures circadian disruption through the average probability that participants are in the same sleep-wake state 24 hours apart, this study examined whether associations between the day-to-day regularity of sleep-wake timing and mortality differ by sex.
Methods
The study included UK Biobank participants with week-long accelerometer-derived sleep-wake data. To reduce reverse causality bias, deaths within one year of recordings were excluded. SRI was calculated by sleepreg. All-cause and CVD mortality were ascertained from inpatient hospital records and death registrars. Age-adjusted Cox proportional hazards models estimated adjusted hazards ratios (aHRs) between SRI categories and time to all-cause or CVD mortality without and with SRI × sex interaction term. SRI–sex combinations were compared using estimated marginal means.
Results
Among 73,647 adults (41,489 [56.3%] female, mean age 62.5±7.8 y) followed for a mean of 7.5±0.9 y, there were 2631 deaths; 20.5% were from primarily CVD causes. Higher age-adjusted mortality rates were observed with the lowest SRI (<60) compared to the highest (≥90) for both all-cause (aHR=2.4; 95% CI=2.0–2.9) and CVD mortality (3.2; 2.1–4.6) (Fig 1). Significant interaction terms were identified for SRI <60 × male (all-cause) and SRI 60–69 × male (CVD). Higher all-cause and CVD mortality rates were associated among males with SRI <60 versus ≥90 (all-cause 2.9; 2.1–4.0; CVD 3.8; 1.9–7.5) and compared to females with SRI <60 (all-cause 2.1; 1.5–3.0; CVD 2.5; 1.2–5.0) (Fig 2). In contrast, neither all-cause nor CVD mortality differed by sex among individuals with SRI ≥90.
Conclusion
Higher mortality rates associated with highly irregular sleep-wake timing are particularly pronounced among males, especially for CVD mortality. The absence of sex differences among those with high sleep regularity suggests that consistent sleep-wake patterns may attenuate heightened male mortality rates.
More abstracts on this topic:
A Quarter Century of Mortality Trends in Hypertension and Sick Sinus Syndrome Among Elderly in the United States
Eltawansy Sherif, Khan Muhammad, Iqbal Asad, Sharif Aleena, Hossain Mohammad, Ali Muhammad Faizan, Ahmad Husnain, Faizan Muhammad, Ahmed Ashraf, Abdul Malik Mohammad Hamza Bin, Pahwani Ritesh, Patel Rahul, Mehdi Hassan
25-Year Decline in Aortic Aneurysm and Dissection Mortality in the U.S.: Impact of Endovascular Repair and Forecast to 2030Ali Manzer, Umar Haddaya, Nazir Tahira, Nizam Muhammad, Steafo Lark, Sharif Ayesha, Jehangir Hanzala, Arham Muhammad, Hamza Anfal, Hassan Arbaz, Amjad Ans, Ali Iman, Zuha Zuha