Final ID: MP179
Cardiorenal Syndrome Type 1 complicated by Uremic Pericarditis and Small Pericardial Effusion causing Cardiac Tamponade
Abstract Body (Do not enter title and authors here): Introduction/Background
Cardiac tamponade is typically associated with large pericardial effusions; however, even small effusions can result in significant hemodynamic compromise, particularly in the setting of rapid fluid accumulation and underlying cardiac pathology. Uremic pericarditis is a rare but serious complication of advanced kidney dysfunction which can progress to tamponade in non-dialyzed patients. We present a case of a elderly man with complex cardiovascular and renal comorbidities who developed obstructive shock from cardiac tamponade despite a small pericardial effusion. This case highlights the diagnostic challenge of recognizing tamponade physiology when classic echocardiographic findings are absent and emphasizes the need to integrate clinical signs and hemodynamics when standard treatments, like dialysis, are not feasible.
Case Report
A 75-year-old man was admitted for acute heart failure complicated by cardiorenal syndrome requiring diuresis. Pleuritic chest pain and hypotension later developed, prompting upgrade to the ICU. Severe uremia, EKG findings, and a small pericardial effusion on TTE suggested uremic pericarditis. Swan-Ganz catheterization showed diastolic normalization of pressures consistent with tamponade physiology. Pericarditis therapy was initiated with prednisone and colchicine; anticoagulation was stopped. The patient’s clinical status subsequently improved.
Discussion
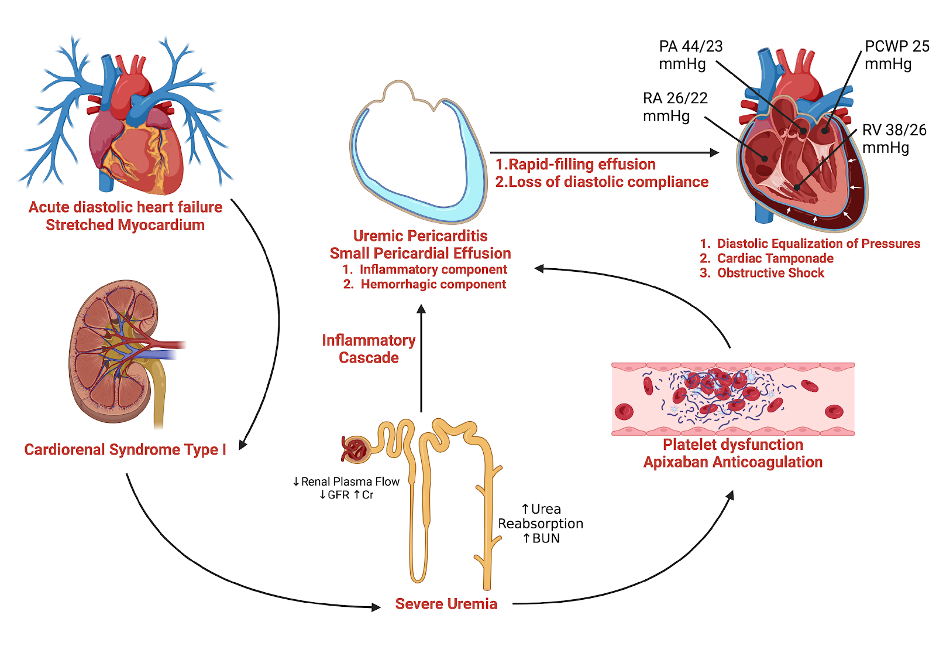
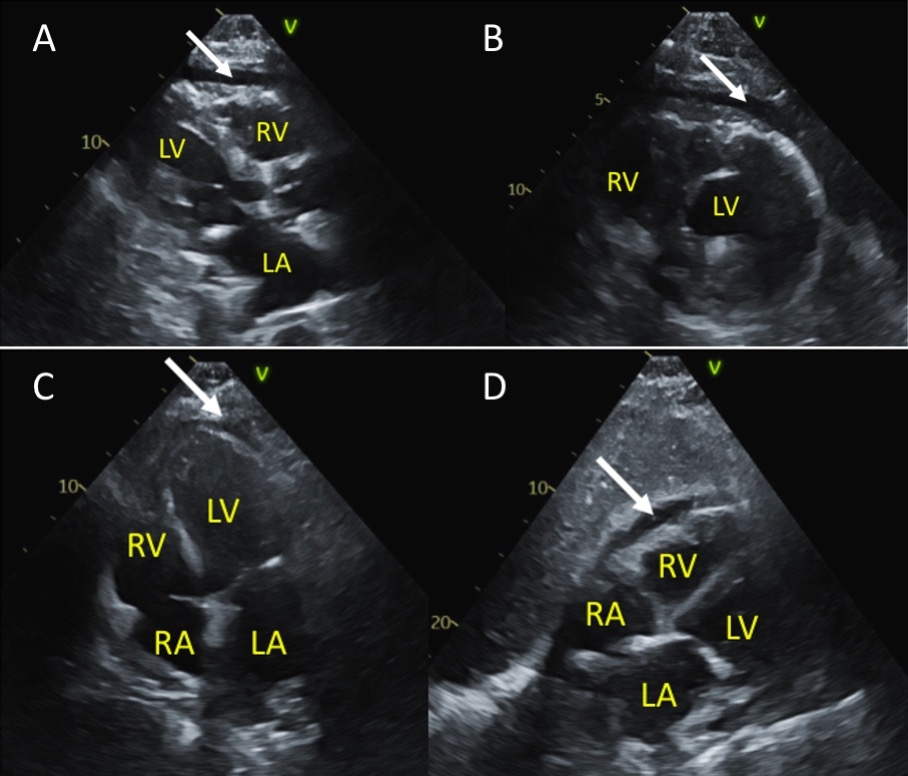
This case illustrates a rare progression from cardiorenal syndrome and uremic pericarditis leading to cardiac tamponade (Fig.1). Despite a small pericardial effusion and lack of classic echocardiographic signs (Fig.2), rapid fluid accumulation likely resulted in tamponade physiology, supported by hemodynamic and clinical findings. Based on ESC guidelines, typical management involves HD. However, successful use of anti-inflammatory treatment in place of dialysis was utilized due to contraindications. Upon readmission, the absence of tamponade signs suggested a slower effusion progression, reinforcing the initial diagnosis of rapid-onset tamponade in a vulnerable myocardium.
Conclusion
This case illustrates the complexity of a small pericardial effusion in the setting of severe uremia and cardiac vulnerability leading to cardiac tamponade. It emphasizes the need for vigilance in recognizing atypical tamponade presentations, while supporting consideration of anti-inflammatory therapy when dialysis cannot be immediately utilized.
Cardiac tamponade is typically associated with large pericardial effusions; however, even small effusions can result in significant hemodynamic compromise, particularly in the setting of rapid fluid accumulation and underlying cardiac pathology. Uremic pericarditis is a rare but serious complication of advanced kidney dysfunction which can progress to tamponade in non-dialyzed patients. We present a case of a elderly man with complex cardiovascular and renal comorbidities who developed obstructive shock from cardiac tamponade despite a small pericardial effusion. This case highlights the diagnostic challenge of recognizing tamponade physiology when classic echocardiographic findings are absent and emphasizes the need to integrate clinical signs and hemodynamics when standard treatments, like dialysis, are not feasible.
Case Report
A 75-year-old man was admitted for acute heart failure complicated by cardiorenal syndrome requiring diuresis. Pleuritic chest pain and hypotension later developed, prompting upgrade to the ICU. Severe uremia, EKG findings, and a small pericardial effusion on TTE suggested uremic pericarditis. Swan-Ganz catheterization showed diastolic normalization of pressures consistent with tamponade physiology. Pericarditis therapy was initiated with prednisone and colchicine; anticoagulation was stopped. The patient’s clinical status subsequently improved.
Discussion
This case illustrates a rare progression from cardiorenal syndrome and uremic pericarditis leading to cardiac tamponade (Fig.1). Despite a small pericardial effusion and lack of classic echocardiographic signs (Fig.2), rapid fluid accumulation likely resulted in tamponade physiology, supported by hemodynamic and clinical findings. Based on ESC guidelines, typical management involves HD. However, successful use of anti-inflammatory treatment in place of dialysis was utilized due to contraindications. Upon readmission, the absence of tamponade signs suggested a slower effusion progression, reinforcing the initial diagnosis of rapid-onset tamponade in a vulnerable myocardium.
Conclusion
This case illustrates the complexity of a small pericardial effusion in the setting of severe uremia and cardiac vulnerability leading to cardiac tamponade. It emphasizes the need for vigilance in recognizing atypical tamponade presentations, while supporting consideration of anti-inflammatory therapy when dialysis cannot be immediately utilized.
More abstracts on this topic:
Acculturation and Cardiovascular-Kidney-Metabolic Syndrome: a Study of Immigrant Adults From the National Health and Nutrition Examination Survey
Chakrabarti Amit, Le Austin, Elfassy Tali, Yang Eugene
A Rare Manifestation of Drug-Induced Lupus: Hydralazine-Induced ANCA Vasculitis and Persistent PericarditisSaini Ishveen, Vo Phuong Uyen, Slabic Andrew, Varian Kenneth