Final ID: MP1471
High Use of P2Y12 Inhibitors and DOACs Persists up to One Year After Percutaneous Left Atrial Appendage Occlusion
Abstract Body (Do not enter title and authors here): Background: Percutaneous left atrial appendage occlusion (pLAAO) is used as an alternative to anticoagulation in patients with atrial fibrillation. Long-term patterns of antiplatelets and anticoagulants use post pLAAO compared to direct oral anticoagulants (DOACs) users are unknown.
Hypothesis: We hypothesized that the use of antiplatelets and anticoagulants remains prevalent up to one year following pLAAO.
Methods: We emulated a target trial where patients with atrial fibrillation were randomly assigned to receive pLAAO or DOACs in the 1:3 ratio using a nationally representative 15% sample of Medicare beneficiaries from Jan 2015 to Dec 2020. We reported the number of patients who received related treatment (>=1 prescription) in the certain time range. We assessed the following drugs up to one year post pLAAO implantation: Antiplatelets (clopidogrel, ticagrelor, prasugrel), 2- vitamin K antagonists (warfarin) and 3- DOACs (apixaban, dabigatran, rivaroxaban, edoxaban).
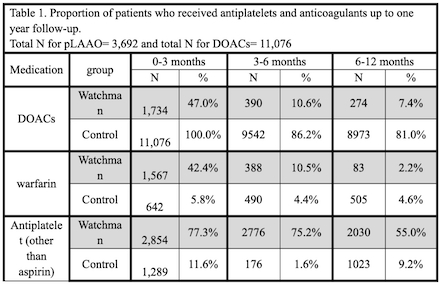
Results: Among 3,692 patients who underwent pLAAO, use of DOACs and warfarin decreased substantially by 6-12 months post pLAAO (from 47.0% to 7.4% and from 42.4% to 2.2%, respectively). In the DOACs arm which had 11,076 patients, use of DOACs remained high on follow up (81.0% at 1-year). At 6-12 months post index date, patients who received pLAAO were significantly less likely to remain on DOACs (7.4% vs. 81.0%; p< 0.001) or warfarin (2.2% vs 4.6%; p < 0.001), but more likely to be on a P2Y12 inhibitor (55.0% vs 9.2%; p < 0.001), table 1.
Conclusion: The use of P2Y12 inhibitors and DOACs remained high at 6-12 months post pLAAO with approximately 1 in 2 patients receiving a prescription for a P2Y12 inhibitor and 1 in 14 receiving a prescription for a DOAC. These high prescribing patterns warrant further investigation as they may be contributing to an increased bleeding risk post pLAAO.
Hypothesis: We hypothesized that the use of antiplatelets and anticoagulants remains prevalent up to one year following pLAAO.
Methods: We emulated a target trial where patients with atrial fibrillation were randomly assigned to receive pLAAO or DOACs in the 1:3 ratio using a nationally representative 15% sample of Medicare beneficiaries from Jan 2015 to Dec 2020. We reported the number of patients who received related treatment (>=1 prescription) in the certain time range. We assessed the following drugs up to one year post pLAAO implantation: Antiplatelets (clopidogrel, ticagrelor, prasugrel), 2- vitamin K antagonists (warfarin) and 3- DOACs (apixaban, dabigatran, rivaroxaban, edoxaban).
Results: Among 3,692 patients who underwent pLAAO, use of DOACs and warfarin decreased substantially by 6-12 months post pLAAO (from 47.0% to 7.4% and from 42.4% to 2.2%, respectively). In the DOACs arm which had 11,076 patients, use of DOACs remained high on follow up (81.0% at 1-year). At 6-12 months post index date, patients who received pLAAO were significantly less likely to remain on DOACs (7.4% vs. 81.0%; p< 0.001) or warfarin (2.2% vs 4.6%; p < 0.001), but more likely to be on a P2Y12 inhibitor (55.0% vs 9.2%; p < 0.001), table 1.
Conclusion: The use of P2Y12 inhibitors and DOACs remained high at 6-12 months post pLAAO with approximately 1 in 2 patients receiving a prescription for a P2Y12 inhibitor and 1 in 14 receiving a prescription for a DOAC. These high prescribing patterns warrant further investigation as they may be contributing to an increased bleeding risk post pLAAO.
More abstracts on this topic:
A randomized controlled trial of antithrombotic therapy in ischemic stroke patients with non-valvular atrial fibrillation and atherosclerosis: The ATIS-NVAF trial
Okazaki Shuhei, Uchida Kazutaka, Asakura Koko, Omae Katsuhiro, Yamamoto Haruko, Hirano Teruyuki, Toyoda Kazunori, Iguchi Yasuyuki, Noguchi Teruo, Okada Yasushi, Kitagawa Kazuo, Tanaka Kanta, Sakai Nobuyuki, Yamagami Hiroshi, Yazawa Yukako, Doijiri Ryosuke, Koga Masatoshi, Ihara Masafumi, Yamamoto Shiro, Kamiyama Kenji, Honda Yuko
Antithrombotic Strategies for Stroke Prevention in Elderly Patients with Atrial Fibrillation: A Meta-Analysis of Contemporary EvidenceFarooq Talha, Pandit Maleeha, Ali Mohammad Eisa, Ahsan Muhammad, Khan Abdul Moiz, Qasim Muhammad, Qayyum Mahhum, Akram Anusha, Kamel Mohammed, Naseem Ali