Final ID: MP196
Safety and Effectiveness of Metabolic and Bariatric Procedures in Heart Failure: A Single-Center Cohort Study
Abstract Body (Do not enter title and authors here): Background: Metabolic and bariatric procedures are associated with reduced heart failure (HF) incidence among individuals with obesity, but studies evaluating their safety and effectiveness in persons with obesity and established HF are scarce.
Aims: To explore the safety and effectiveness of metabolic and bariatric procedures, including surgical and endoscopic interventions, among individuals with and without HF.
Methods: In this single-center retrospective cohort study spanning 2021-2023, persons with HF in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) were identified using external adjudication criteria. Our primary objective was to examine 30-day safety outcomes by HF status. Secondary objectives included the evaluation of temporal changes in body weight (baseline to 30 days and 1 year) and changes in medication use between (baseline to 1 year).
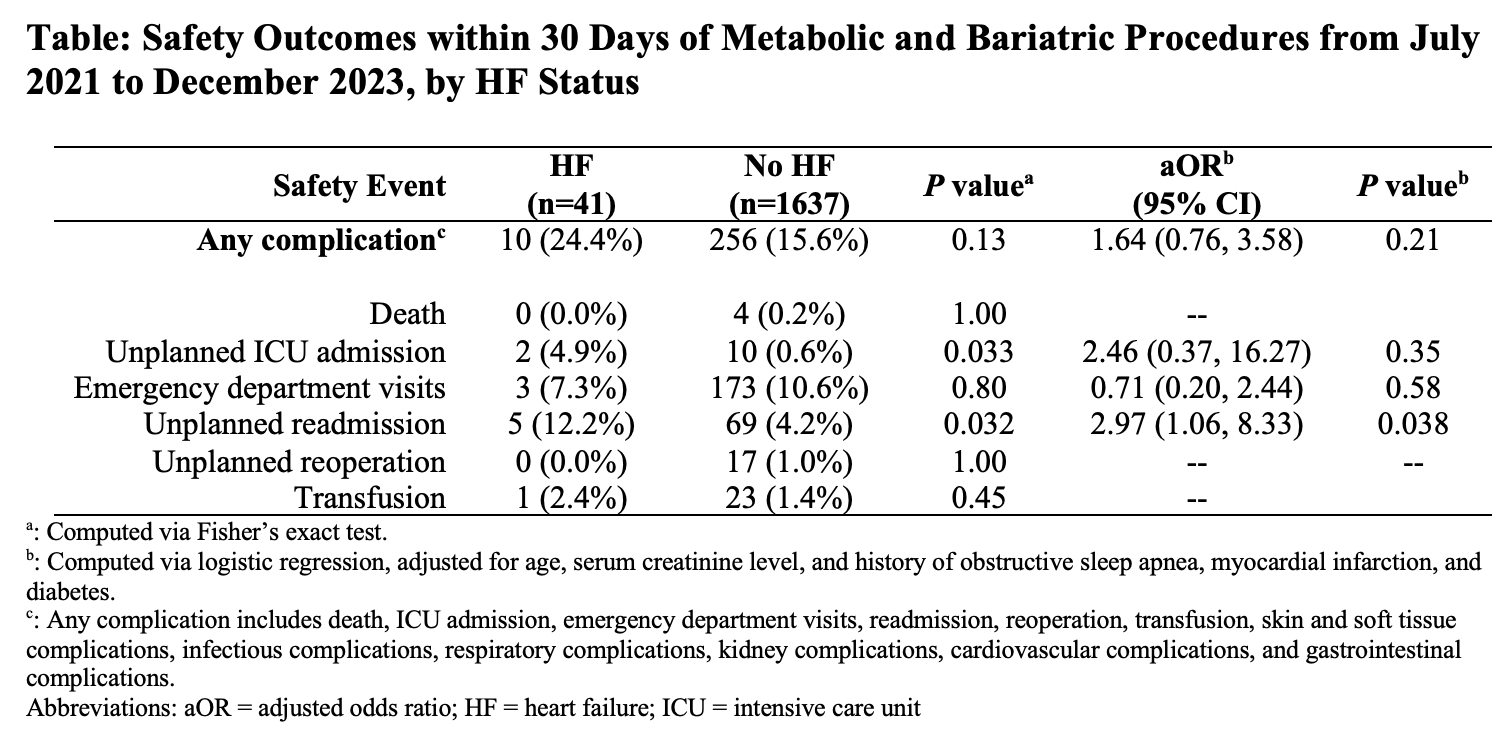
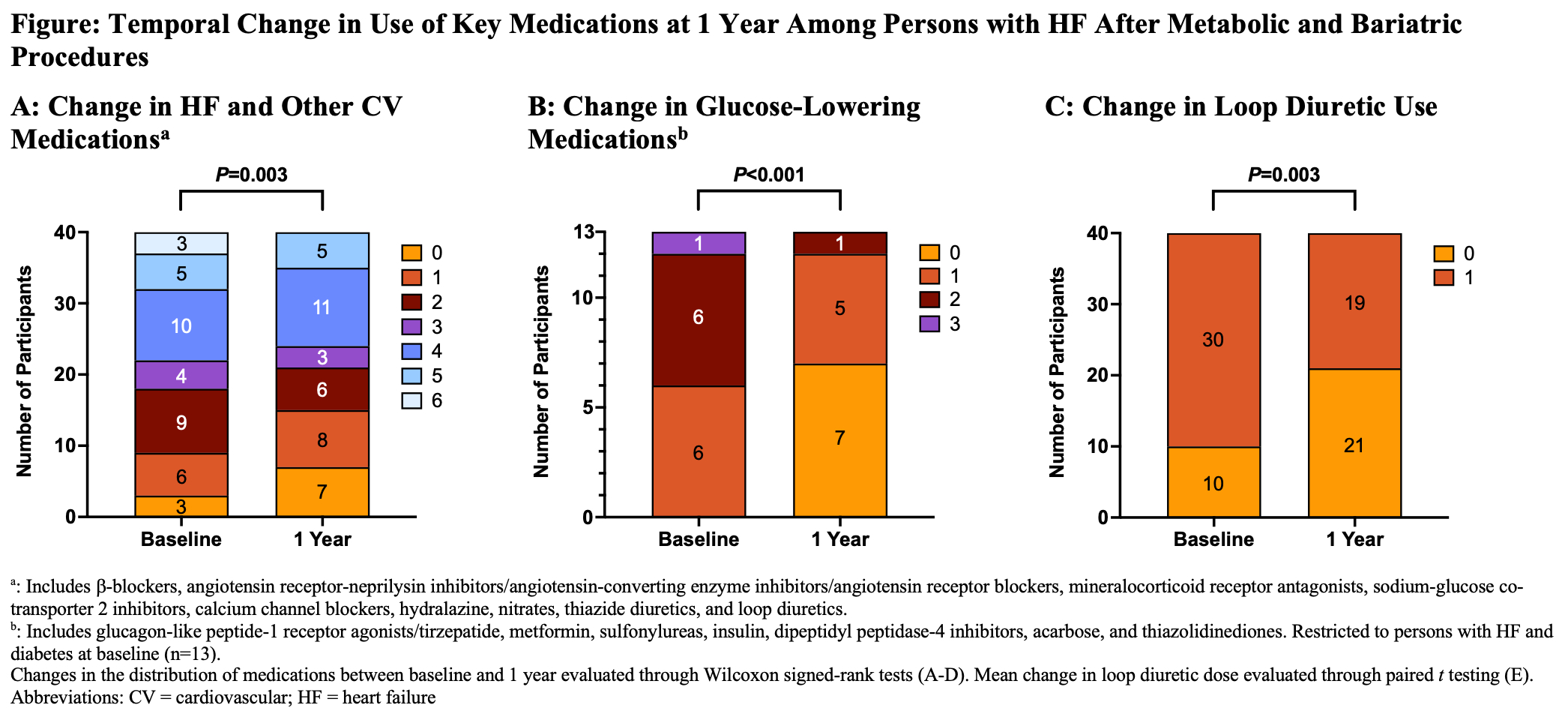
Results: Among 1,678 metabolic and bariatric procedures conducted over the study period (mean age, 43±12 years; 86% female; mean body mass index [BMI], 42±8 kg/m2), 41 (2.4%) were performed in persons with HF. The most common (80%) index metabolic and bariatric procedure in HF was laparoscopic sleeve gastrectomy. Compared with persons without HF, those with HF tended to have older age, male sex, higher BMI, worse kidney function, and a greater burden of obesity-related complications. Persons with HF did not appear to experience higher risk of any 30-day complication vs. those without HF (24% vs. 16%; adjusted odds ratio [aOR], 1.64; 95% CI, 0.76 to 3.58; P=0.21) (Table). There were no instances of death at 30 days among persons with HF. However, HF was associated with higher odds of unplanned readmission (aOR, 2.97; 95% CI, 1.06 to 8.33; P=0.038). Overall, 30-day change in body weight was similar between those with (-5.9%; 95% CI, -6.9 to -4.9%) and without HF (-6.2%; 95% CI, -6.4 to -6.0%; P=0.57). By 1-year, individuals with HF experienced significant reductions in body weight (mean change, -18.7%; 95% CI, -22.1 to -15.3%; P<0.001), HF and other cardiovascular medications (P=0.003), glucose-lowering medications (P<0.001), and loop diuretics (P=0.003) (Figure).
Conclusions: These findings suggest that metabolic and bariatric procedures are safe and effective among persons with obesity and established HF, and may inform future prospective studies in this population.
Aims: To explore the safety and effectiveness of metabolic and bariatric procedures, including surgical and endoscopic interventions, among individuals with and without HF.
Methods: In this single-center retrospective cohort study spanning 2021-2023, persons with HF in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) were identified using external adjudication criteria. Our primary objective was to examine 30-day safety outcomes by HF status. Secondary objectives included the evaluation of temporal changes in body weight (baseline to 30 days and 1 year) and changes in medication use between (baseline to 1 year).
Results: Among 1,678 metabolic and bariatric procedures conducted over the study period (mean age, 43±12 years; 86% female; mean body mass index [BMI], 42±8 kg/m2), 41 (2.4%) were performed in persons with HF. The most common (80%) index metabolic and bariatric procedure in HF was laparoscopic sleeve gastrectomy. Compared with persons without HF, those with HF tended to have older age, male sex, higher BMI, worse kidney function, and a greater burden of obesity-related complications. Persons with HF did not appear to experience higher risk of any 30-day complication vs. those without HF (24% vs. 16%; adjusted odds ratio [aOR], 1.64; 95% CI, 0.76 to 3.58; P=0.21) (Table). There were no instances of death at 30 days among persons with HF. However, HF was associated with higher odds of unplanned readmission (aOR, 2.97; 95% CI, 1.06 to 8.33; P=0.038). Overall, 30-day change in body weight was similar between those with (-5.9%; 95% CI, -6.9 to -4.9%) and without HF (-6.2%; 95% CI, -6.4 to -6.0%; P=0.57). By 1-year, individuals with HF experienced significant reductions in body weight (mean change, -18.7%; 95% CI, -22.1 to -15.3%; P<0.001), HF and other cardiovascular medications (P=0.003), glucose-lowering medications (P<0.001), and loop diuretics (P=0.003) (Figure).
Conclusions: These findings suggest that metabolic and bariatric procedures are safe and effective among persons with obesity and established HF, and may inform future prospective studies in this population.
More abstracts on this topic:
A Case of Dilated Cardiomyopathy and Systemic Thromboembolism in a Young Patient on Testosterone Replacement Therapy
Sabri Muhammad, Ijaz Naila, Nadeem Ramsha, Checchio Lucy, Riaz Faiza
Long-Term Impact of Bariatric Surgery on Hypertension Control and Remission: A Meta-Analysis of Randomized Controlled TrialsSebastian Sneha Annie, Shah Yash, Krishnamoorthy Geetha