Final ID: HCM6
Right Ventricular Role in Heart Failure of Mildly Symptomatic and Asymptomatic Patients with Obstructive Hypertrophic Cardiomyopathy
Abstract Body (Do not enter title and authors here): Background
Heart failure (HF) is the most common complication in patients with obstructive hypertrophic cardiomyopathy (oHCM), significantly impairing quality of life and prognosis. In asymptomatic or mildly symptomatic patients, reliable markers for HF progression are lacking. Early identification could improve counseling and support timely consideration of gradient-reducing therapies. Although potentially important, the role of the right ventricle (RV) in HF progression in oHCM remains poorly understood. This study evaluated RV parameters by cardiac magnetic resonance (CMR) as early predictors of HF risk beyond conventional metrics in oHCM.
Methods
In a multi-center cohort of 3134 patients with HCM who underwent CMR between 2003 and 2023, we identified 771 mildly or asymptomatic (NYHA I/II) patients with oHCM, rest or provoked gradients ≥30 mmHg, LVEF ≥50%, and no prior septal reduction therapy (SRT). CMR-derived biventricular volumes were indexed to BSA, LGE was manually quantified. The primary outcome was a composite “HF Event”: progression to NYHA Class III/IV, SRT, new LVEF<50%, HF-related death, or heart transplantation. To further investigate predictors of newly emerging HF symptoms, a secondary analysis was performed in the subgroup of 347 asymptomatic patients (NYHA class I), using the composite endpoint “HF Progression”: new HF symptoms (NYHA class ≥II), SRT, new LVEF<50%, HF-related death, or heart transplantation. Uni and multivariable Cox regression analyses were performed, and Kaplan–Meier plots visualize the prognostic relevance of RV stroke volume index (SVI) at an optimal cutoff determined by Youden’s index.
Results
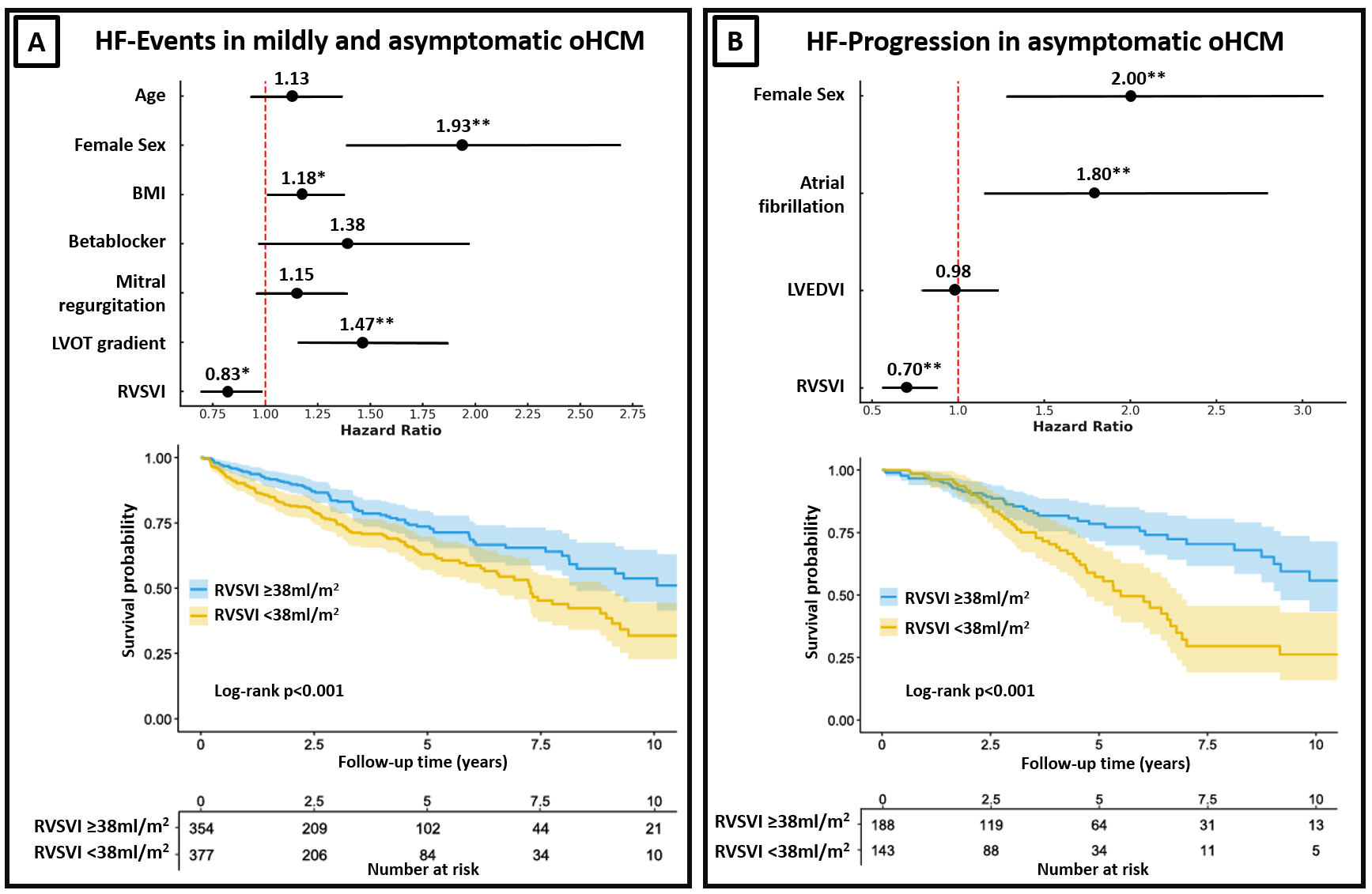
Over a mean follow-up of 3.6±3.0 years, 216 (28%) patients experienced HF Events. These patients were older, more often female, had higher BMI and outflow gradients, more intense medical treatment, and smaller RV volumes and RVSVI (Table 1). In regression analyses, lower RVSVI emerged as an independent predictor of HF Events (Figure 1A). Among asymptomatic patients, 98 (28%) experienced HF Progression over a mean follow-up of 4.0±3.0years. Female sex, atrial fibrillation, and lower RVSVI were independent predictors of HF progression in this subgroup (Figure 1B).
Conclusion
In oHCM patients with no or mild symptoms, lower RVSVI emerged as an independent predictor of future HF symptoms and adverse HF events. These findings highlight the underrecognized prognostic relevance of the RV in oHCM.
Heart failure (HF) is the most common complication in patients with obstructive hypertrophic cardiomyopathy (oHCM), significantly impairing quality of life and prognosis. In asymptomatic or mildly symptomatic patients, reliable markers for HF progression are lacking. Early identification could improve counseling and support timely consideration of gradient-reducing therapies. Although potentially important, the role of the right ventricle (RV) in HF progression in oHCM remains poorly understood. This study evaluated RV parameters by cardiac magnetic resonance (CMR) as early predictors of HF risk beyond conventional metrics in oHCM.
Methods
In a multi-center cohort of 3134 patients with HCM who underwent CMR between 2003 and 2023, we identified 771 mildly or asymptomatic (NYHA I/II) patients with oHCM, rest or provoked gradients ≥30 mmHg, LVEF ≥50%, and no prior septal reduction therapy (SRT). CMR-derived biventricular volumes were indexed to BSA, LGE was manually quantified. The primary outcome was a composite “HF Event”: progression to NYHA Class III/IV, SRT, new LVEF<50%, HF-related death, or heart transplantation. To further investigate predictors of newly emerging HF symptoms, a secondary analysis was performed in the subgroup of 347 asymptomatic patients (NYHA class I), using the composite endpoint “HF Progression”: new HF symptoms (NYHA class ≥II), SRT, new LVEF<50%, HF-related death, or heart transplantation. Uni and multivariable Cox regression analyses were performed, and Kaplan–Meier plots visualize the prognostic relevance of RV stroke volume index (SVI) at an optimal cutoff determined by Youden’s index.
Results
Over a mean follow-up of 3.6±3.0 years, 216 (28%) patients experienced HF Events. These patients were older, more often female, had higher BMI and outflow gradients, more intense medical treatment, and smaller RV volumes and RVSVI (Table 1). In regression analyses, lower RVSVI emerged as an independent predictor of HF Events (Figure 1A). Among asymptomatic patients, 98 (28%) experienced HF Progression over a mean follow-up of 4.0±3.0years. Female sex, atrial fibrillation, and lower RVSVI were independent predictors of HF progression in this subgroup (Figure 1B).
Conclusion
In oHCM patients with no or mild symptoms, lower RVSVI emerged as an independent predictor of future HF symptoms and adverse HF events. These findings highlight the underrecognized prognostic relevance of the RV in oHCM.
More abstracts on this topic:
A Dangerous Right Turn: Primary Right Heart Failure in Mechanically Ventilated Patients—-Prevalence, Inpatient Outcomes, and High Use of Advanced ICU Therapies— A Nationwide Analysis
Khan Dawlat, Chaudhry Hammad, Shehzad Dawood, Riaz Muhammad Faisal, Ahmed Mamoon
A Multicenter Friedreich Ataxia Registry Identifies Posterior Wall Thickness as a Predictor of Major Adverse Cardiac EventsLin Kimberly, Johnson Jonathan, Mccormack Shana, Lynch David, Tate Barbara, Feng Yixuan, Huang Jing, Mercer-rosa Laura, Dedio Anna, Mcsweeney Kara, Fournier Anne, Yoon Grace, Payne Ronald, Cripe Linda, Patel Aarti, Niaz Talha