Final ID: MP2249
Mandatory Use of the Least Expensive ACEis and ARBs Would Generate Significant Cost Savings Within Medicare Part D
Abstract Body (Do not enter title and authors here):
Introduction
Serving more than 50 million beneficiaries, Medicare Part D has a responsibility to balance broad prescription drug coverage with fiscal sustainability. We provide an up-to-date assessment of expenditures and cost-saving opportunities within the program, focusing on angiotensin-converting enzyme inhibitors (ACEis) and angiotensin II receptor blockers (ARBs)—common cardiovascular drugs with many generic and brand-name options.
Objectives
To describe trends in utilization and spending on ACEis and ARBs among Part D beneficiaries. To model potential savings from substituting (a) every brand-name prescription with therapeutically-equivalent generics, or (b) every prescription with the least expensive generic in each drug class.
Methods
This retrospective cross-sectional study analyzed the latest Medicare Part D public use files, containing prescription drug expenditure data from 2018 to 2022. Single-ingredient ACEis and ARBs were extracted, with combination products excluded. Outcomes were total beneficiary count, annual expenditure, spending per beneficiary, cost per dosage unit (CPDU), and potential savings to Medicare Part D. All monetary values were inflation-adjusted to 2022 dollars.
Results
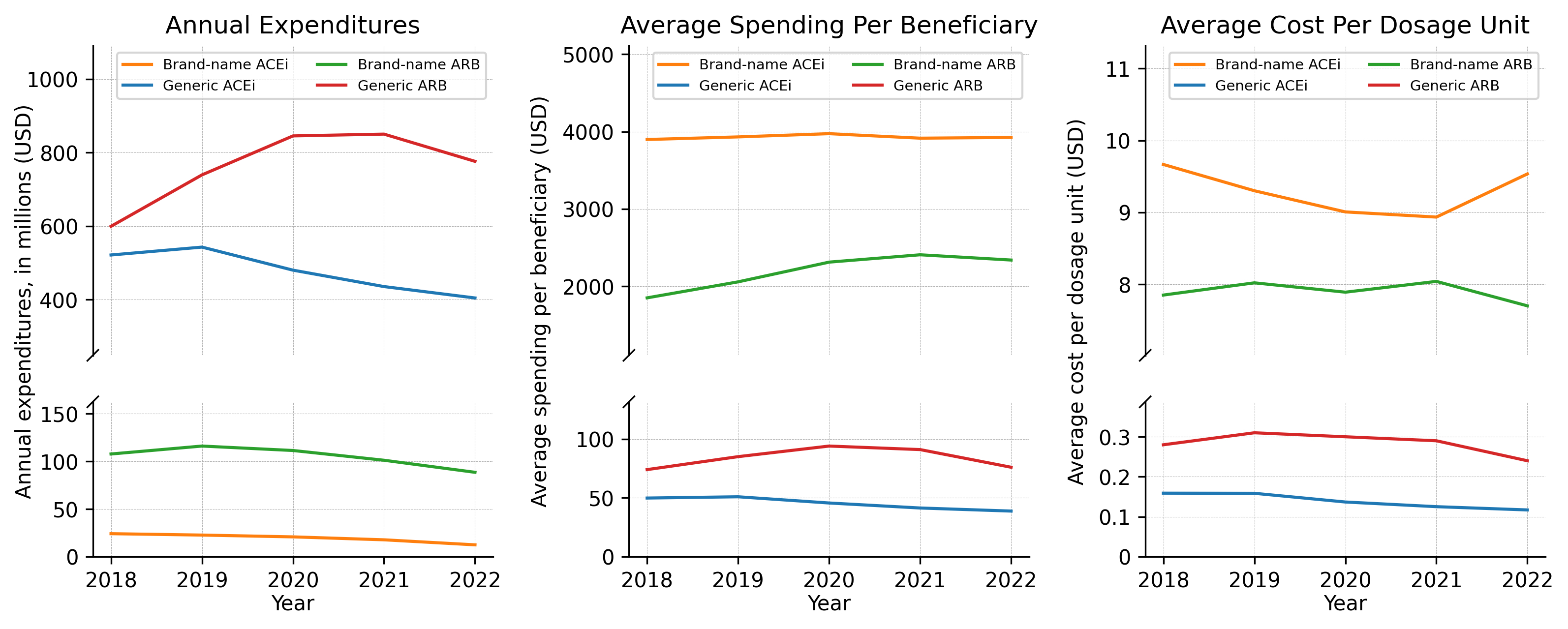
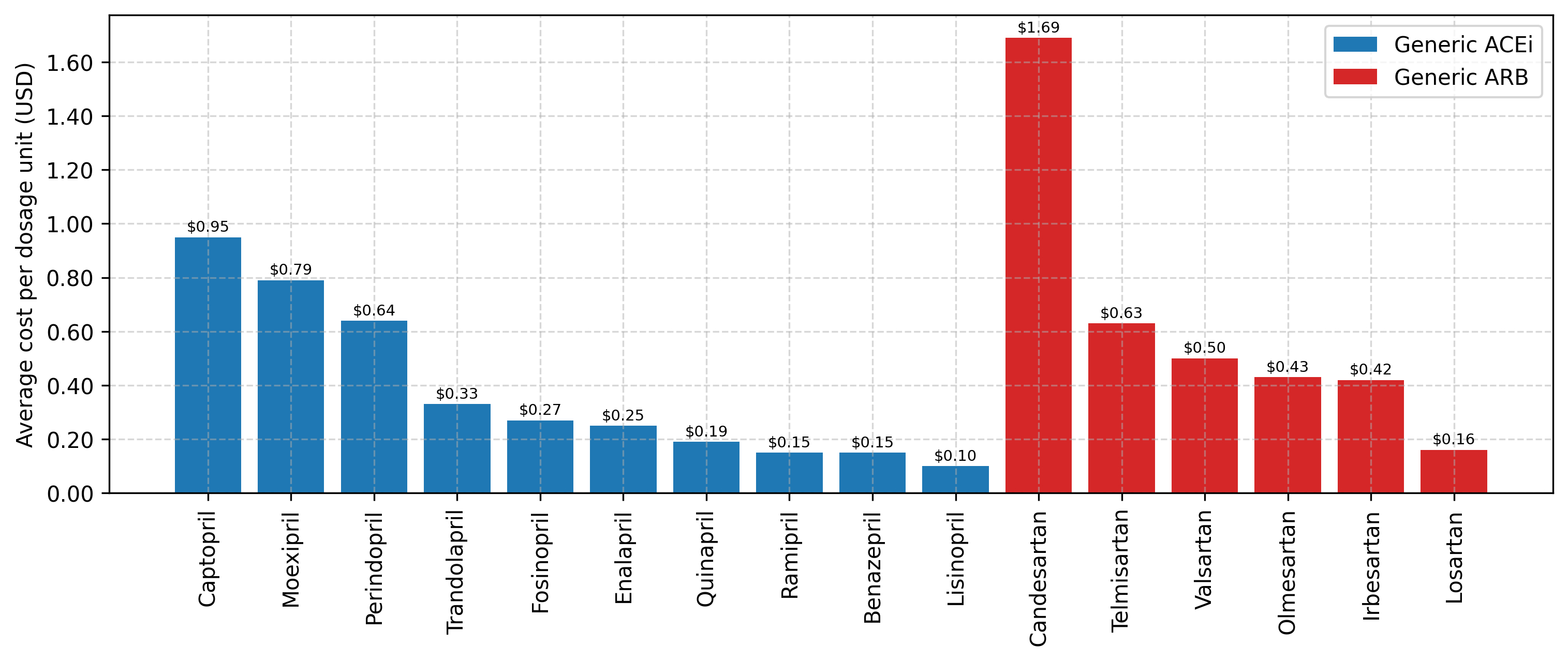
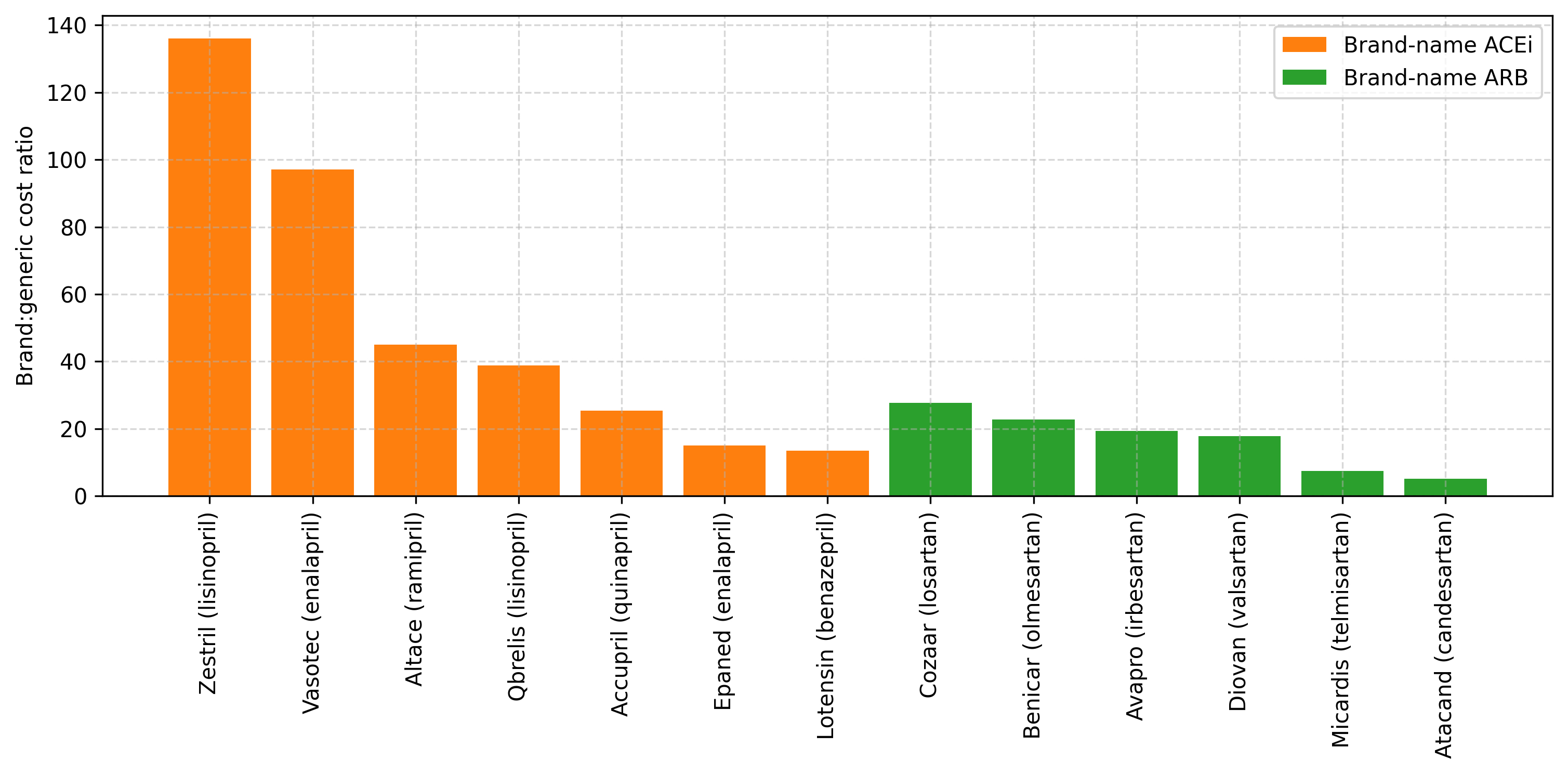
Between 2018 and 2022, the number of Medicare Part D enrollees increased from 44,249,461 to 50,305,097 (+13.7%). While the number prescribed an ACEi or ARB rose from 18,625,796 to 20,643,466 (+10.8%), the rate per 10,000 beneficiaries fell from 4,209 to 4,104 (−2.51%). Annual expenditures on these drugs grew from $1.25 billion in 2018 to $1.28 billion in 2022 (+2.30%). CPDU of brand-names remained largely unchanged (ACEis: −1.36%; ARBs: −1.98%), while generics saw a price reduction (ACEis: −26.4%; ARBs: −13.3%). Over the years studied, we estimated potential cumulative savings of (a) $429 million with complete generic substitution, and (b) $2.66 billion if all prescriptions were converted to the cheapest generic in each drug class.
Limitations
The data set aggregated spending metrics for all drug strengths and excluded manufacturer rebates. Savings estimate (b) assumes therapeutic interchangeability between drugs of the same class.
Conclusion
Our analysis shows that substantial savings are possible with both (a) complete generic substitution, and (b) mandatory use of the least costly generic formulation of two commonly prescribed drug classes. Comparable opportunities likely exist for other widely-prescribed drugs and warrants further investigation.
Introduction
Serving more than 50 million beneficiaries, Medicare Part D has a responsibility to balance broad prescription drug coverage with fiscal sustainability. We provide an up-to-date assessment of expenditures and cost-saving opportunities within the program, focusing on angiotensin-converting enzyme inhibitors (ACEis) and angiotensin II receptor blockers (ARBs)—common cardiovascular drugs with many generic and brand-name options.
Objectives
To describe trends in utilization and spending on ACEis and ARBs among Part D beneficiaries. To model potential savings from substituting (a) every brand-name prescription with therapeutically-equivalent generics, or (b) every prescription with the least expensive generic in each drug class.
Methods
This retrospective cross-sectional study analyzed the latest Medicare Part D public use files, containing prescription drug expenditure data from 2018 to 2022. Single-ingredient ACEis and ARBs were extracted, with combination products excluded. Outcomes were total beneficiary count, annual expenditure, spending per beneficiary, cost per dosage unit (CPDU), and potential savings to Medicare Part D. All monetary values were inflation-adjusted to 2022 dollars.
Results
Between 2018 and 2022, the number of Medicare Part D enrollees increased from 44,249,461 to 50,305,097 (+13.7%). While the number prescribed an ACEi or ARB rose from 18,625,796 to 20,643,466 (+10.8%), the rate per 10,000 beneficiaries fell from 4,209 to 4,104 (−2.51%). Annual expenditures on these drugs grew from $1.25 billion in 2018 to $1.28 billion in 2022 (+2.30%). CPDU of brand-names remained largely unchanged (ACEis: −1.36%; ARBs: −1.98%), while generics saw a price reduction (ACEis: −26.4%; ARBs: −13.3%). Over the years studied, we estimated potential cumulative savings of (a) $429 million with complete generic substitution, and (b) $2.66 billion if all prescriptions were converted to the cheapest generic in each drug class.
Limitations
The data set aggregated spending metrics for all drug strengths and excluded manufacturer rebates. Savings estimate (b) assumes therapeutic interchangeability between drugs of the same class.
Conclusion
Our analysis shows that substantial savings are possible with both (a) complete generic substitution, and (b) mandatory use of the least costly generic formulation of two commonly prescribed drug classes. Comparable opportunities likely exist for other widely-prescribed drugs and warrants further investigation.
More abstracts on this topic:
Burden of Non-Rheumatic Valvular Heart Disease in High-income Asia Pacific from 1990-2019: A Benchmarking analysis
Shaikh Salomi, Amin Vishrant, Desai Hardik, Sharma Kamal, Shandilya Ashwinikumar, Patel Khushbu, Waqas Muhammad, Syed Saif, Lakkimsetti Mohit, Bhalodia Paritaben, Islam Hamza, Patel Juhi
Cardiology Medications and Medicare Spending: Opportunities for Savings Using Mark Cuban Cost Plus Drug Company and Costco Member Prescription Program PricingSchoeffler Katherine, Day Stephanie, Sanjamala Hemanth, Danesh Alireza, Rosales Isaac, Fennell Zachary, Aguilar Atticus, Parikh Suparshva, Nipp Ryan