Final ID: Su1033
ST-Elevation Myocardial Infarction (STEMI) and Rhabdomyolysis: Analyzing In-Hospital Outcomes using the National Inpatient Sample
Abstract Body (Do not enter title and authors here): Introduction:
Rhabdomyolysis is reported in approximately 25,000 cases annually in the United States. The demographic characteristics, clinical outcomes, and health care utilization of individuals with and without rhabdomyolysis who have had an ST-elevation myocardial infarction (STEMI) have not yet been the subject of any large, nationwide studies.
Methods:
The United States National inpatient sample (2018-2020) was analyzed to identify hospitalized patients with STEMI with and without rhabdomyolysis using ICD-10 codes. Confounders were adjusted by using multivariable regression analysis. The primary outcome of our study was in-hospital mortality, and the secondary outcomes were mean length of stay (LOS), mean total hospital charge (THC), incidence of acute kidney injury, hyponatremia, hyperkalemia, renal replacement therapy, acute respiratory failure, cardiac arrhythmias, heart failure, venous thromboembolism, and cardiac arrest.
Results:
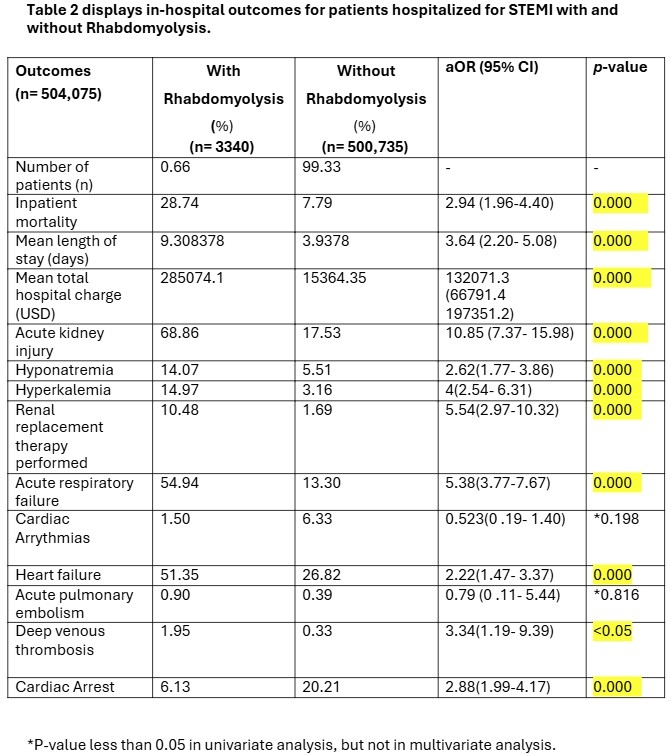
Out of 504,075 hospitalized patients with STEMI, 3340 (0.66%) had rhabdomyolysis, and 500,735 (99.33 %) were without rhabdomyolysis. Patients with STEMI who also developed rhabdomyolysis were found to have 4-fold increase in inpatient mortality (adjusted Odds ratio [aOR] 2.94; 95% confidence interval [CI], 1.96-4.40; p <0.001), with an adjusted increase in mean length of stay of 3.64 (95% confidence interval [CI], 2.20- 5.08; p <0.001),and an adjusted increase in mean total hospital charges of 132071.3 (95% confidence interval [CI], 66791.4-197351.2; p<0.001). Rate of acute kidney injury and renal replacement therapy increased 4 and 5-fold respectively (p < 0.001). Similarly, rate of hyponatremia, hyperkalemia, acute respiratory failure, heart failure, and cardiac arrest were all significantly higher in the rhabdomyolysis group (all p < 0.001).
The incidence of DVT was high in the rhabdomyolysis group (p < 0.05), however, no statistically significant difference in of rates of acute pulmonary embolism, and cardiac arrhythmias was observed between the two groups.
Conclusions:
Rhabdomyolysis in STEMI patients could be precipitated by skeletal muscle hypoxia. Our study showed significantly increased mortality, length of hospital stays, total hospital charge, and rate of various system-based complications in subgroup of STEMI patients who also developed rhabdomyolysis. More research is required to further investigate this association.
Rhabdomyolysis is reported in approximately 25,000 cases annually in the United States. The demographic characteristics, clinical outcomes, and health care utilization of individuals with and without rhabdomyolysis who have had an ST-elevation myocardial infarction (STEMI) have not yet been the subject of any large, nationwide studies.
Methods:
The United States National inpatient sample (2018-2020) was analyzed to identify hospitalized patients with STEMI with and without rhabdomyolysis using ICD-10 codes. Confounders were adjusted by using multivariable regression analysis. The primary outcome of our study was in-hospital mortality, and the secondary outcomes were mean length of stay (LOS), mean total hospital charge (THC), incidence of acute kidney injury, hyponatremia, hyperkalemia, renal replacement therapy, acute respiratory failure, cardiac arrhythmias, heart failure, venous thromboembolism, and cardiac arrest.
Results:
Out of 504,075 hospitalized patients with STEMI, 3340 (0.66%) had rhabdomyolysis, and 500,735 (99.33 %) were without rhabdomyolysis. Patients with STEMI who also developed rhabdomyolysis were found to have 4-fold increase in inpatient mortality (adjusted Odds ratio [aOR] 2.94; 95% confidence interval [CI], 1.96-4.40; p <0.001), with an adjusted increase in mean length of stay of 3.64 (95% confidence interval [CI], 2.20- 5.08; p <0.001),and an adjusted increase in mean total hospital charges of 132071.3 (95% confidence interval [CI], 66791.4-197351.2; p<0.001). Rate of acute kidney injury and renal replacement therapy increased 4 and 5-fold respectively (p < 0.001). Similarly, rate of hyponatremia, hyperkalemia, acute respiratory failure, heart failure, and cardiac arrest were all significantly higher in the rhabdomyolysis group (all p < 0.001).
The incidence of DVT was high in the rhabdomyolysis group (p < 0.05), however, no statistically significant difference in of rates of acute pulmonary embolism, and cardiac arrhythmias was observed between the two groups.
Conclusions:
Rhabdomyolysis in STEMI patients could be precipitated by skeletal muscle hypoxia. Our study showed significantly increased mortality, length of hospital stays, total hospital charge, and rate of various system-based complications in subgroup of STEMI patients who also developed rhabdomyolysis. More research is required to further investigate this association.
More abstracts on this topic:
ATTR-CM in the U.S.: Patterns of Healthcare Use and Medical Costs
Kim Sodam, Shah Kanya, Didomenico Robert, Winn Aaron
A Case of Myocardial Infarction with Non-obstructive Coronary Arteries (MINOCA) Complicated by a Ventricular Septal Defect (VSD)Thai Theresa, Lipinski Jerry, Sola Michael, El Rafei Abdelghani, Desai Aken, Sailer Christine