Final ID: MP779
Impact of adverse events on clinical outcomes in patients with cardiogenic shock supported by temporary mechanical circulatory support devices
Aim: To assess whether DRAEs are associated with worse in-hospital outcomes in patients with CS.
Methods: A retrospective chart review was conducted to identify patients with CS requiring tMCS at the Medical University of South Carolina from 8/2021 to 8/2023. Patients were stratified by presence/absence of a DRAE (occurring while on tMCS support or ≤48 hrs of tMCS removal). DRAE definitions were based on published guidelines and included bacteremia, bleeding, neurologic event, vascular injury, heparin induced thrombocytopenia and hemolysis. Outcomes included in-hospital death and “unfavorable outcome” (death prior to heart transplant, durable LVAD, or discharge). Multivariable logistic regression was performed to account for differences in baseline characteristics.
Results: Among 268 patients included, 112 (41.8%) had a DRAE and 156 (58.2%) did not. The median (25th, 75th) age was 60 (44, 67) years, 36.6% were Black, and 28.4% were female (p=NS between groups). Historical atrial fibrillation (AF) and HFrEF were more common in those with a DRAE than those without (34.0% vs 22.3%, p=0.04 for AF; 73.7% vs 54.5%, p<0.01 for HFrEF). Those with a DRAE had more advanced CS (stage D/E 72.3% vs 50.0%, p<0.01), more commonly had cardiac arrest prior to tMCS (23.2% v 9.6%, p<0.01), and more commonly were on ECMO (33.9% v 5.1%, p<0.01).
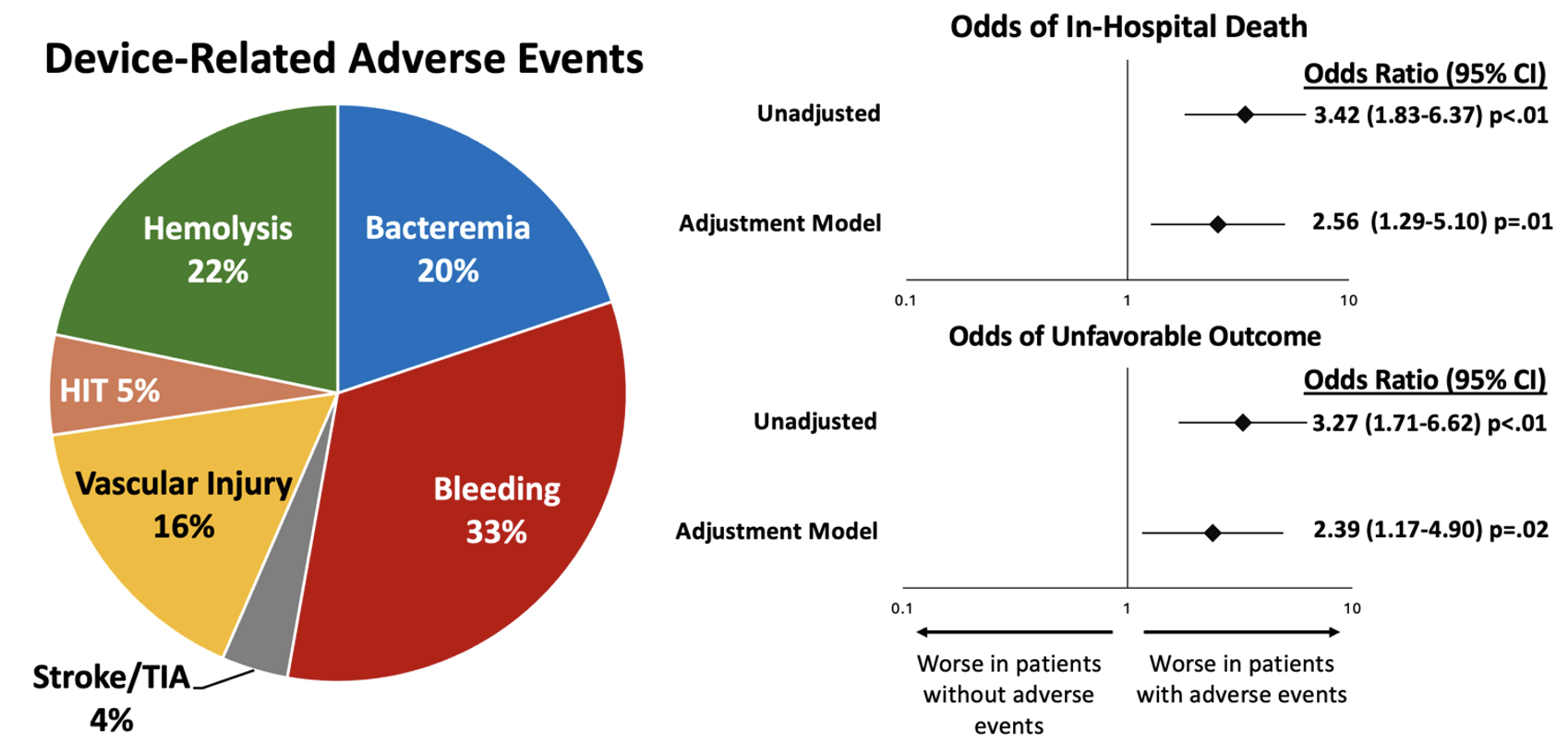
The median hospital length of stay was 30 (18, 46) days, with no significant difference between groups. In the DRAE group, a total of 161 unique DRAEs occurred, with 48 patients experiencing >1 DRAE. The most common AE was bleeding, followed by hemolysis, and bacteremia (Figure). In-hospital death was more common in the DRAE group (32.1% vs 12.2%; unadjusted OR [95% CI] 3.42 [1.83-6.37]; p<0.01). Unfavorable outcome was also more common in the DRAE group (28.6% vs 10.9%, unadjusted OR 3.27 [1.71-6.26]; p<0.01) (Figure). These findings were consistent after adjustment for age, sex, history of HFrEF, history of AF, and ECMO exposure.
Conclusion: The presence of a DRAE in patients with CS and tMCS is associated with a significantly higher in-hospital mortality and unfavorable outcome.
- Samani, Stephanie ( MUSC , Charleston , South Carolina , United States )
- Silkowski, Molly ( MUSC , Charleston , South Carolina , United States )
- Dodson, Kaylen ( MUSC , Charleston , South Carolina , United States )
- Bull, Lindsey ( MUSC , Charleston , South Carolina , United States )
- Hajj, Jennifer ( MUSC , Charleston , South Carolina , United States )
- Gregoski, Mathew ( MUSC , Charleston , South Carolina , United States )
- Tedford, Ryan ( MUSC , Charleston , South Carolina , United States )
- Mcmurray, Jeff ( MUSC , Charleston , South Carolina , United States )
- Witer, Lucas ( MUSC , Charleston , South Carolina , United States )
- Kilic, Arman ( MUSC , Charleston , South Carolina , United States )
- Houston, Brian ( MUSC , Charleston , South Carolina , United States )
- Patel, Zachary ( MUSC , Charleston , South Carolina , United States )
- Carnicelli, Anthony ( MUSC , Charleston , South Carolina , United States )
- Ospina, Meg ( MUSC , Charleston , South Carolina , United States )
- Mittelstaedt, Roxanne ( MUSC , Charleston , South Carolina , United States )
- Peller, Jacob ( MUSC , Charleston , South Carolina , United States )
- Marchell, Charlotte ( MUSC , Charleston , South Carolina , United States )
- Ohlrich, Kelly ( MUSC , Charleston , South Carolina , United States )
- Gunn, Brady ( MUSC , Charleston , South Carolina , United States )
- Varrone, Michael ( MUSC , Charleston , South Carolina , United States )
Meeting Info:
Session Info:
Crash and Burn: Cardiogenic Shock Clinical Science
Saturday, 11/08/2025 , 03:15PM - 04:25PM
Moderated Digital Poster Session
More abstracts on this topic:
Wozniak Phillip, Grodzinsky Anna
6-Nitrodopamine potentiates the positive chronotopic and inotropic effect induced by noradrenaline in the rat isolated heartLima Antonio, Sobanski Joao Fernando, Antunes Edson, De Nucci Gilberto
More abstracts from these authors:
Patel Zachary, Silkowski Molly, Dodson Kaylen, Bull Lindsey, Gregoski Mathew, Tedford Ryan, Mcmurray Jeffrey, Witer Lucas, Kilic Arman, Houston Brian, Carnicelli Anthony, Ospina Meg, Mittelstaedt Roxanne, Peller Jacob, Samani Stephanie, Marchell Charlotte, Ohlrich Kelly, Gunn Brady, Varrone Michael
Clinical management of select patients with surgically implanted Impella 5.5 left ventricular assist devices on a cardiovascular step-down unitOspina Meg, Bull Lindsey, Inampudi Chakradhari, Mcmurray Jeff, Tedford Ryan, Witer Lucas, Bhandari Krishna, Yourshaw Jeffrey, Houston Brian, Kilic Arman, Carnicelli Anthony, Griffin Jan, Van Bakel Adrian, Jackson Gregory, Rao Vishal N., Atkins Jessica, Hajj Jennifer, Dodson Kaylen, Summer Mary Kathryn