Final ID: MP829
Comparison of Clinical Outcomes of DOACs versus Warfarin in patients with nonischemic HFrEF and HFpEF: A Retrospective Cohort Study
Abstract Body (Do not enter title and authors here): Background: The incidence, management, and outcomes of left ventricular (LV) thrombus in nonischemic cardiomyopathy (NICM) remain poorly defined.
Research question: Do outcomes differ between DOACs and warfarin in treating LV thrombus in patients with HFrEF or HFpEF secondary to NICM?
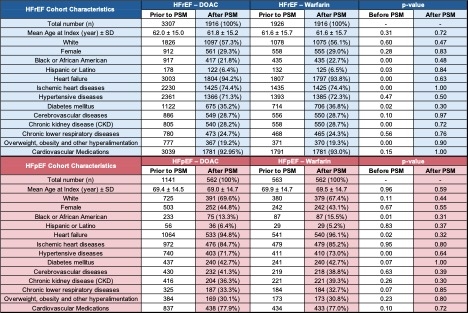
Methods: This retrospective cohort study utilized data from the TriNetX database. Patients diagnosed with HFrEF or HFpEF not secondary to ischemic disease with subsequent left ventricular thrombus, between December 1, 2004 and December 1, 2024, were included. Propensity score matching (PSM) was performed on all data to account for differences in potential confounding variables (Table 1). Subgroup analyses compared outcomes for patients anticoagulated with a DOAC versus warfarin after diagnosis of LV thrombus. Primary outcomes of stroke, major bleeding, systemic embolism, and all-cause mortality were assessed at 3 months, 6 months, 1 year, and 2 years after initiation of anticoagulation using risk and Kaplan–Meier survival analysis.
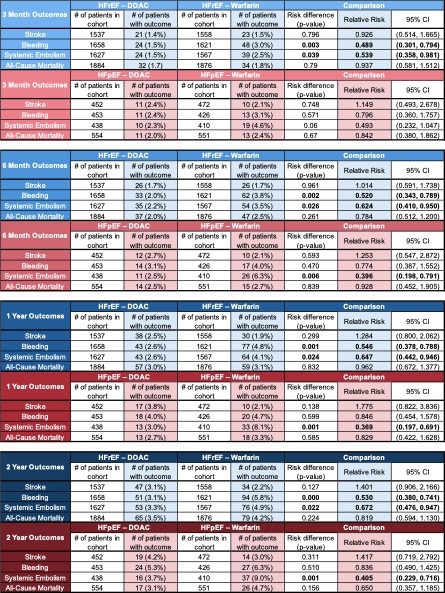
Results: The study included 1,916 HFrEF patients and 562 HFpEF patients. Among HFrEF patients, DOAC treatment compared to warfarin was associated with a lower incidence of systemic embolism at all time points: 3 months (relative risk [RR] 0.04; 95% confidence interval [CI] (0.36-0.98, p = 0.04)), 6 months (RR 0.62 (CI 0.41-0.95, p = 0.03)), 1 year (RR 0.65 (CI 0.44-0.95, p = 0.02)), and 2 years (RR 0.67 (CI 0.48-0.95, p = 0.02)) and lower risk of bleeding at 3 months (RR 0.49 (CI 0.30-0.79, p < 0.01)), 6 months (RR 0.52 (CI, 0.34-0.79, p < 0.01)), 1 year (RR 0.55 (CI 0.38-0.79, p < 0.01)), and 2 years (RR 0.53 (CI 0.38-0.74, p < 0.01)). There were no significant differences in the risk of stroke or all-cause mortality at any time point. Among HFpEF patients, DOAC treatment compared to warfarin was associated with a lower incidence of systemic embolism at 6 months (RR 0.40 (CI 0.20-0.79, p < 0.01)), 1 year (RR 0.37 (CI 0.20-0.69, p < 0.01)), and 2 years (RR 0.41 (CI, 0.23-0.72, p < 0.01)). There were no significant differences in the risk of stroke, bleeding, or all-cause mortality at any time point (Table 2).
Conclusions: In NICM patients with HFrEF or HFpEF and LV thrombus, DOACs were associated with reduced risk of systemic embolism and bleeding, compared to warfarin. These findings support the consideration of DOACs as a preferred anticoagulation strategy in this population.
Research question: Do outcomes differ between DOACs and warfarin in treating LV thrombus in patients with HFrEF or HFpEF secondary to NICM?
Methods: This retrospective cohort study utilized data from the TriNetX database. Patients diagnosed with HFrEF or HFpEF not secondary to ischemic disease with subsequent left ventricular thrombus, between December 1, 2004 and December 1, 2024, were included. Propensity score matching (PSM) was performed on all data to account for differences in potential confounding variables (Table 1). Subgroup analyses compared outcomes for patients anticoagulated with a DOAC versus warfarin after diagnosis of LV thrombus. Primary outcomes of stroke, major bleeding, systemic embolism, and all-cause mortality were assessed at 3 months, 6 months, 1 year, and 2 years after initiation of anticoagulation using risk and Kaplan–Meier survival analysis.
Results: The study included 1,916 HFrEF patients and 562 HFpEF patients. Among HFrEF patients, DOAC treatment compared to warfarin was associated with a lower incidence of systemic embolism at all time points: 3 months (relative risk [RR] 0.04; 95% confidence interval [CI] (0.36-0.98, p = 0.04)), 6 months (RR 0.62 (CI 0.41-0.95, p = 0.03)), 1 year (RR 0.65 (CI 0.44-0.95, p = 0.02)), and 2 years (RR 0.67 (CI 0.48-0.95, p = 0.02)) and lower risk of bleeding at 3 months (RR 0.49 (CI 0.30-0.79, p < 0.01)), 6 months (RR 0.52 (CI, 0.34-0.79, p < 0.01)), 1 year (RR 0.55 (CI 0.38-0.79, p < 0.01)), and 2 years (RR 0.53 (CI 0.38-0.74, p < 0.01)). There were no significant differences in the risk of stroke or all-cause mortality at any time point. Among HFpEF patients, DOAC treatment compared to warfarin was associated with a lower incidence of systemic embolism at 6 months (RR 0.40 (CI 0.20-0.79, p < 0.01)), 1 year (RR 0.37 (CI 0.20-0.69, p < 0.01)), and 2 years (RR 0.41 (CI, 0.23-0.72, p < 0.01)). There were no significant differences in the risk of stroke, bleeding, or all-cause mortality at any time point (Table 2).
Conclusions: In NICM patients with HFrEF or HFpEF and LV thrombus, DOACs were associated with reduced risk of systemic embolism and bleeding, compared to warfarin. These findings support the consideration of DOACs as a preferred anticoagulation strategy in this population.
More abstracts on this topic:
A Silent Storm: Incidental Discovery of IVC and Right Atrium Thrombus in a Patient with Uterine Stromal Sarcoma
Wasef Natale, Fatima Tehreem, Stys Adam
A Unique STEMI Etiology: Paradoxical Coronary EmbolismDavis Thomas, Saado Jonathan, Kietrsunthorn Patrick, Williams Eric