Final ID: MP635
Regional Differences in Outcomes in Adults after Percutaneous Coronary Intervention (PCI) for Stable Ischemic Heart Disease
Abstract Body (Do not enter title and authors here): Background:
Previous studies on Percutaneous Coronary Intervention (PCI) for Acute Coronary Syndrome (ACS) have found a disparate distribution of healthcare resources across U.S. regions, contributing to regional differences in cardiovascular outcomes. Whether regional variation in clinical outcomes exist among patients with Chronic Coronary Disease (CCD) who undergo PCI remains unknown.
Research question: Does regional variation affect clinical outcomes in patients with chronic coronary disease undergoing percutaneous coronary intervention in the United States?
Methods:
We included patients undergoing PCI for CCD between January 2016 and June 2022 using the Vizient® Clinical Database. We evaluated major adverse cardiovascular events (MACE) — encompassing in-hospital all-cause mortality, myocardial infarction (MI), or repeat coronary revascularization by PCI or CABG — across hospitals in the South, Northeast, Midwest, and West within one year of the index PCI. We also assessed secondary outcomes, including individual components of the composite, major bleeding, and cardiovascular-related hospitalizations. We adjusted for demographics, comorbidities, hospital characteristics, encounter information, and procedural information.
Results:
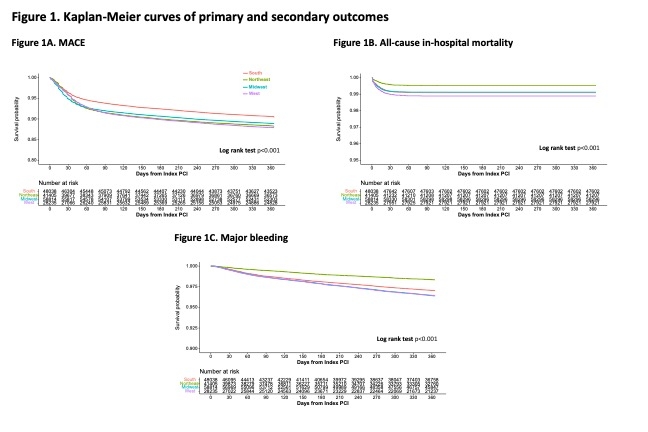
A total of 176,492 patients were included across 176 hospitals, with 22% of patients from hospitals in the South, 23.46% Northeast, 33.32% Midwest, and 16% from the West. When compared with hospitals in the South as the reference, all other regions had higher risk of MACE and repeat PCI (Figure 1). After adjusting for covariates, patients cared for in Midwest hospitals had a higher risk of MACE (relative risk [RR] 1.24, 95% Confidence Interval [CI] 1.19-1.30), all-cause in-hospital mortality (RR 1.25, 95% CI 1.09-1.43), MI (RR 1.37, 95% CI 1.24-1.51), major bleeding(RR 1.33, 95% CI 1.23-1.44), cardiovascular-related hospitalizations (RR 1.04, 95% CI 1.01-1.08), renal replacement therapy (RR 1.41, 95% CI 1.19-1.66), and repeat PCI (RR 1.21, 95% CI 1.15-1.27). In contrast, patients in the Northeast had the lowest relative risk of mortality (RR 0.69, 95% CI 0.57-0.84) and major bleeding (RR 0.72, 95% CI 0.64-0.81).
Conclusion:
Significant regional variation exists in clinical outcomes following PCI in patients with CCD. Understanding driving factors for these disparities represents a target for future quality improvement efforts.
Previous studies on Percutaneous Coronary Intervention (PCI) for Acute Coronary Syndrome (ACS) have found a disparate distribution of healthcare resources across U.S. regions, contributing to regional differences in cardiovascular outcomes. Whether regional variation in clinical outcomes exist among patients with Chronic Coronary Disease (CCD) who undergo PCI remains unknown.
Research question: Does regional variation affect clinical outcomes in patients with chronic coronary disease undergoing percutaneous coronary intervention in the United States?
Methods:
We included patients undergoing PCI for CCD between January 2016 and June 2022 using the Vizient® Clinical Database. We evaluated major adverse cardiovascular events (MACE) — encompassing in-hospital all-cause mortality, myocardial infarction (MI), or repeat coronary revascularization by PCI or CABG — across hospitals in the South, Northeast, Midwest, and West within one year of the index PCI. We also assessed secondary outcomes, including individual components of the composite, major bleeding, and cardiovascular-related hospitalizations. We adjusted for demographics, comorbidities, hospital characteristics, encounter information, and procedural information.
Results:
A total of 176,492 patients were included across 176 hospitals, with 22% of patients from hospitals in the South, 23.46% Northeast, 33.32% Midwest, and 16% from the West. When compared with hospitals in the South as the reference, all other regions had higher risk of MACE and repeat PCI (Figure 1). After adjusting for covariates, patients cared for in Midwest hospitals had a higher risk of MACE (relative risk [RR] 1.24, 95% Confidence Interval [CI] 1.19-1.30), all-cause in-hospital mortality (RR 1.25, 95% CI 1.09-1.43), MI (RR 1.37, 95% CI 1.24-1.51), major bleeding(RR 1.33, 95% CI 1.23-1.44), cardiovascular-related hospitalizations (RR 1.04, 95% CI 1.01-1.08), renal replacement therapy (RR 1.41, 95% CI 1.19-1.66), and repeat PCI (RR 1.21, 95% CI 1.15-1.27). In contrast, patients in the Northeast had the lowest relative risk of mortality (RR 0.69, 95% CI 0.57-0.84) and major bleeding (RR 0.72, 95% CI 0.64-0.81).
Conclusion:
Significant regional variation exists in clinical outcomes following PCI in patients with CCD. Understanding driving factors for these disparities represents a target for future quality improvement efforts.
More abstracts on this topic:
A First-in-Class EV-miRNA Diagnostic System for Early Identification of IVIG-Resistant Kawasaki Disease
Nakaoka Hideyuki, Hirono Keiichi, Hara Akane, Tsuboi Kaori, Ibuki Keijiro, Ozawa Sayaka, Ichida Fukiko
Non-invasive Algorithmic Hemodynamic Measurements Using Wearable Cloth-based Nanotechnology: Alternative to Invasive Right Heart CatheterizationIsath Ameesh, Gass Alan, Khan Shazli, Kanwal Arjun, Gregory Vasiliki, Shyam Kumar Prashanth, Ramasamy Mouli, Varadan Venk, Zimmerman John, Varadan Vijay