Final ID: MP401
Mortality in Cardiac Complications of Heart Disease in the United States (1999–2023): A 25-Year Analysis of Trends and Sociodemographic Disparities from the CDC WONDER Database
Abstract Body (Do not enter title and authors here): Background
Heart disease remains the leading cause of mortality in the U.S., with many patients experiencing life-threatening complications such as ruptured chorda tendinea, papillary muscle rupture, intracardiac thrombosis, and myocardial degeneration. This study examines sociodemographic trends and disparities in mortality from cardiac complications of heart disease among adults aged ≥25 years.
Methods
A retrospective analysis of mortality data from 1999 to 2023 was conducted using the CDC WONDER database. Deaths were identified using ICD-10 code I51 (complications and ill-defined descriptions of heart disease). Age-adjusted mortality rates (AAMRs) per 100,000 persons were calculated and stratified by year, sex, race, ethnicity, and geographic region. Trends were evaluated using Joinpoint regression and expressed as Average Annual Percent Change (AAPC) with 95% confidence intervals (CI); statistical significance was set at p<0.05.
Results
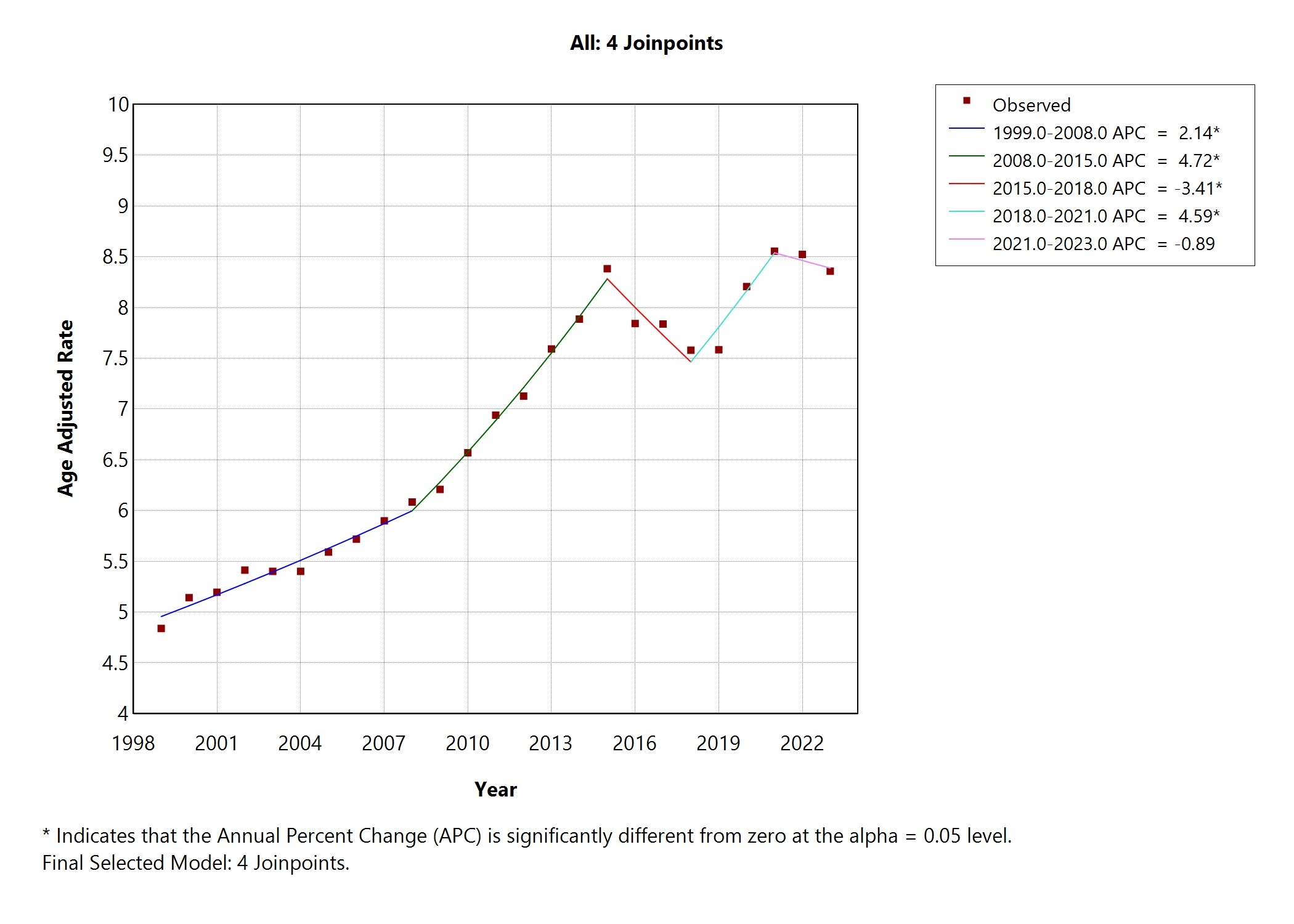
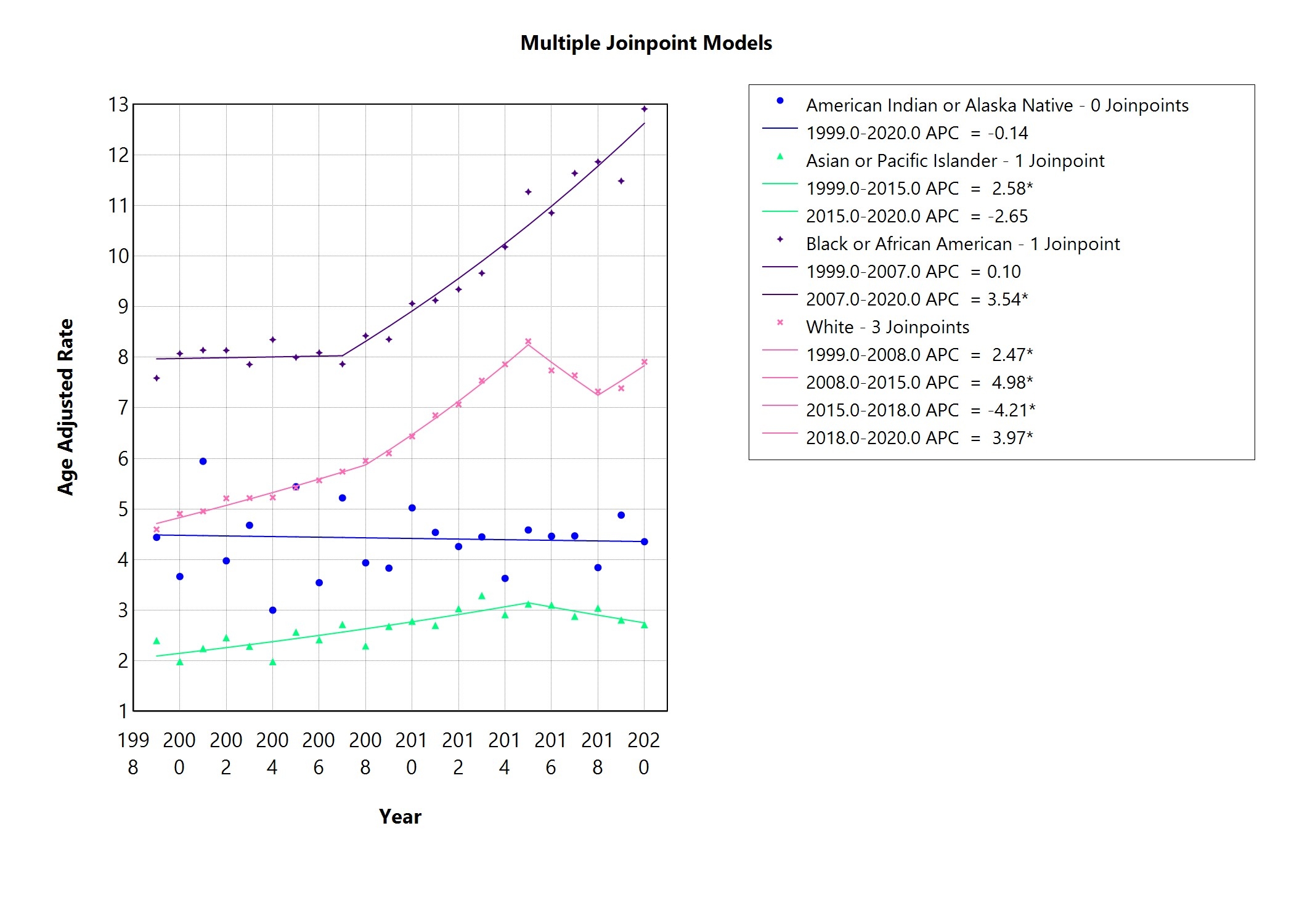
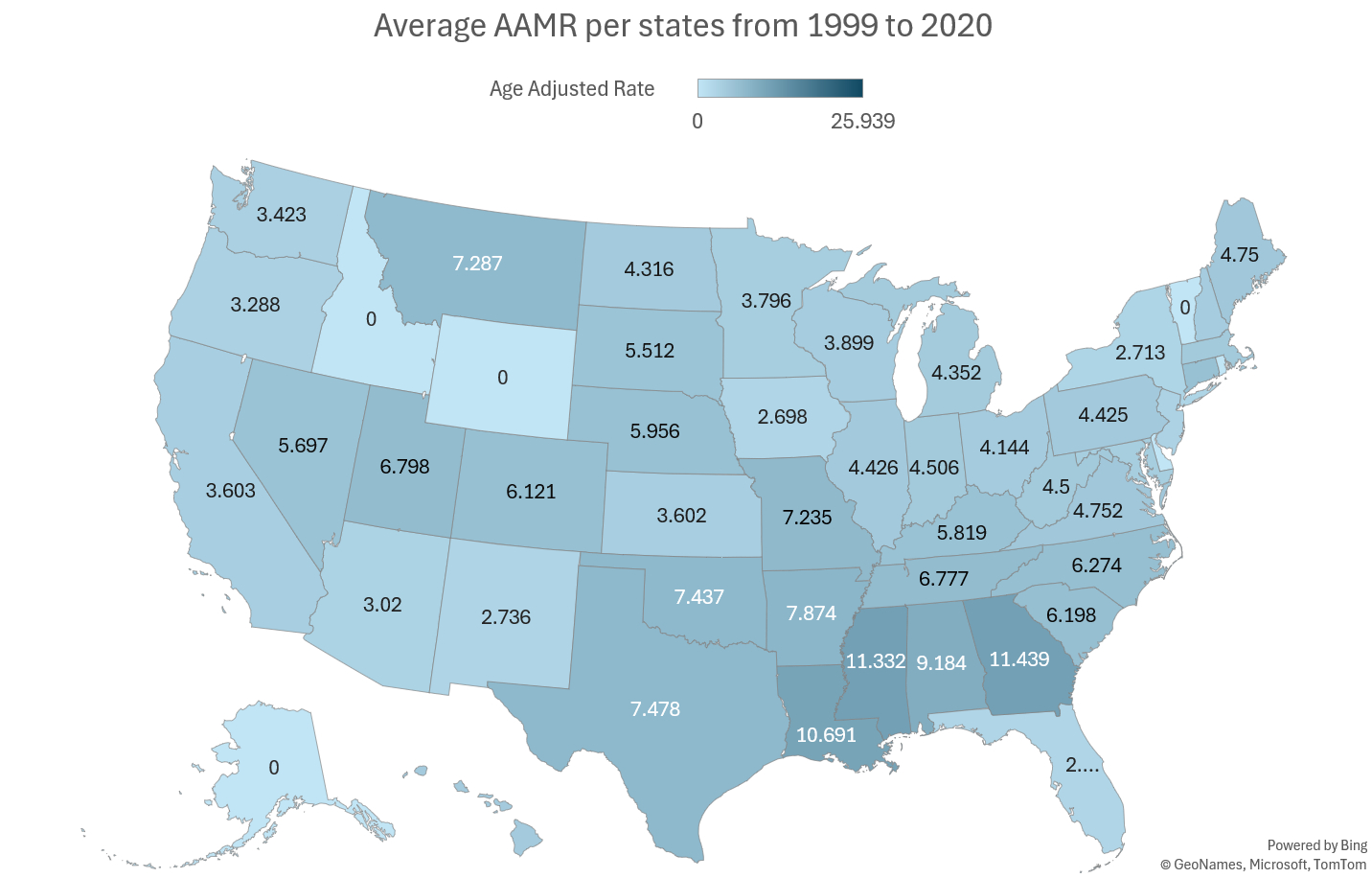
Between 1999 and 2023, 387,197 deaths were attributed to cardiac complications of heart disease. The national AAMR nearly doubled from 4.84 in 1999 to 8.36 in 2023 (AAPC = 2.22%, p<0.0001). Overall trends included: a moderate rise (1999–2008, 2.14%), a steeper increase (2008–2015, 4.72%), a decline (2015–2018, -3.41%), a rebound (2018–2021, 4.49%), and a slight decrease (2021–2023, -0.89%). Males consistently had higher AAMRs than females (8.34 vs. 5.50, p<0.001). Racial and ethnic disparities were notable: Non-Hispanic individuals had a higher AAMR than Hispanic individuals (7.02 vs. 4.49, p<0.0001); Black or African American individuals exhibited the highest rates (ANOVA F(5,30)=224.43, p<0.0001). Regionally, the South had the highest AAMR (9.20), with Georgia having the highest and Washington the lowest state-level rates. Urbanization analysis showed significant variation (ANOVA F(5,126)=11.64, p<0.0001), with NonCore (nonmetro) and Small Metro areas having higher mortality than Large Central Metro areas (8.30 vs. 5.68).
Conclusion
Mortality from cardiac complications of heart disease has markedly increased over the past 25 years, with pronounced disparities by sex, race/ethnicity, region, and urbanization. Men, Black or African American individuals, and residents of the South and small or nonmetro areas are disproportionately affected. These findings highlight the urgent need for targeted interventions to address structural and healthcare access inequities and improve cardiovascular outcomes in high-risk populations.
Heart disease remains the leading cause of mortality in the U.S., with many patients experiencing life-threatening complications such as ruptured chorda tendinea, papillary muscle rupture, intracardiac thrombosis, and myocardial degeneration. This study examines sociodemographic trends and disparities in mortality from cardiac complications of heart disease among adults aged ≥25 years.
Methods
A retrospective analysis of mortality data from 1999 to 2023 was conducted using the CDC WONDER database. Deaths were identified using ICD-10 code I51 (complications and ill-defined descriptions of heart disease). Age-adjusted mortality rates (AAMRs) per 100,000 persons were calculated and stratified by year, sex, race, ethnicity, and geographic region. Trends were evaluated using Joinpoint regression and expressed as Average Annual Percent Change (AAPC) with 95% confidence intervals (CI); statistical significance was set at p<0.05.
Results
Between 1999 and 2023, 387,197 deaths were attributed to cardiac complications of heart disease. The national AAMR nearly doubled from 4.84 in 1999 to 8.36 in 2023 (AAPC = 2.22%, p<0.0001). Overall trends included: a moderate rise (1999–2008, 2.14%), a steeper increase (2008–2015, 4.72%), a decline (2015–2018, -3.41%), a rebound (2018–2021, 4.49%), and a slight decrease (2021–2023, -0.89%). Males consistently had higher AAMRs than females (8.34 vs. 5.50, p<0.001). Racial and ethnic disparities were notable: Non-Hispanic individuals had a higher AAMR than Hispanic individuals (7.02 vs. 4.49, p<0.0001); Black or African American individuals exhibited the highest rates (ANOVA F(5,30)=224.43, p<0.0001). Regionally, the South had the highest AAMR (9.20), with Georgia having the highest and Washington the lowest state-level rates. Urbanization analysis showed significant variation (ANOVA F(5,126)=11.64, p<0.0001), with NonCore (nonmetro) and Small Metro areas having higher mortality than Large Central Metro areas (8.30 vs. 5.68).
Conclusion
Mortality from cardiac complications of heart disease has markedly increased over the past 25 years, with pronounced disparities by sex, race/ethnicity, region, and urbanization. Men, Black or African American individuals, and residents of the South and small or nonmetro areas are disproportionately affected. These findings highlight the urgent need for targeted interventions to address structural and healthcare access inequities and improve cardiovascular outcomes in high-risk populations.
More abstracts on this topic:
A Measurement Model of Socioeconomic Status and its Association with Cardiovascular Disease in the Hispanic Community Health Study/Study of Latinos
Cordero Christina, Llabre Maria, Romaker Emma, Kobayashi Marissa, Gianola Morgan, Gallo Linda, Isasi Carmen, Perreira Krista, Corsino Leonor, Zhou Laura
A Deep Learning Digital Biomarker for Mitral Valve Prolapse using Echocardiogram VideosAl-alusi Mostafa, Khurshid Shaan, Sanborn Danita, Picard Michael, Ho Jennifer, Maddah Mahnaz, Ellinor Patrick, Lau Emily, Small Aeron, Reeder Christopher, Shnitzer Dery Tal, Andrews Carl, Kany Shinwan, Ramo Joel, Haimovich Julian