Final ID: MP1062
The Prevalence of Pulmonary Hypertension in Hypertensive Heart Failure in Sub-Saharan Africa
Abstract Body (Do not enter title and authors here): Background: Elevated blood pressure (BP) presents a major challenge in sub-Saharan (SSA), affecting ~1 in 10 people. The left ventricle (LV) adapts to chronic pressure overload with hypertrophy and later dilation resulting in diastolic and, subsequently, systolic dysfunction, both of which predispose to pulmonary hypertension (PH). When present, PH contributes to decreased quality of life, reduced exercise capacity, and shortened lifespan. To date, no reports on the prevalence of PH in hypertensive heart failure (HHF) exist, but profiling this is a major step toward population health initiatives aimed at mitigating the PH-HHF burden in low-resource regions.
Methods: We conducted a systematic literature search following PRISMA and GATHER guidelines searching PubMed, Embase, Web of Science, and LILACS for studies published until 09/2023 on patients in SSA with diagnosed HHF who underwent echocardiography. HHF was defined as BP>180/100mmHg, accompanied by symptoms of HF, increased LV septal thickness (>13mm), and systolic (LV ejection fraction [EF] <50%) or diastolic (EF≥50% and E/A<1) dysfunction. PH was defined as mild (tricuspid regurgitation velocity [TRV] >2.8m/s) or severe (>3.4m/s). We excluded studies without a clear PH definition and performed a meta-analysis using a random-effects model of proportions. All studies were assessed for risk of bias.
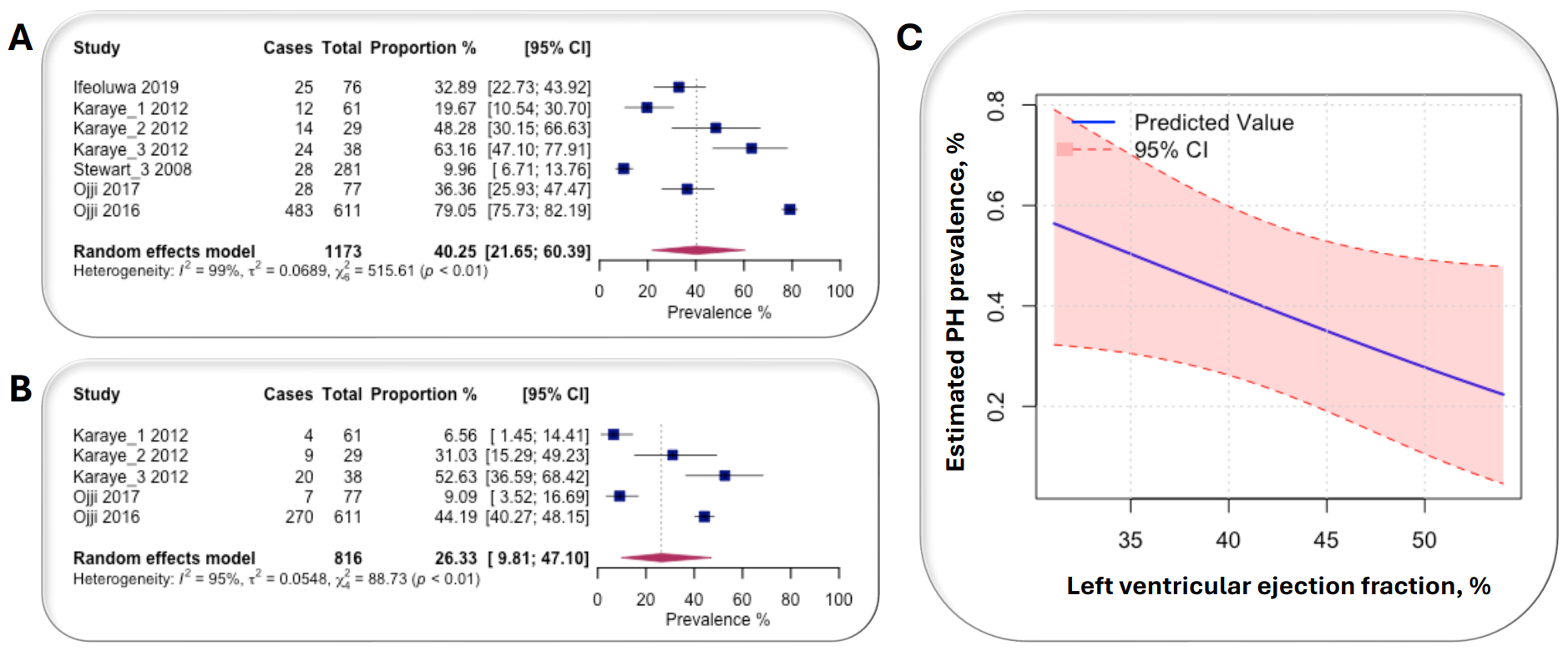
Results: We included N=7 studies, published between 2008–2019, compromising N=1,173 patients (mean age, 54±3 years; male, 53±16%). There were n=3 studies (n=371 patients) and n=4 studies (n=802) that analyzed systolic (mean EF 53±16%) and diastolic (EF 33±15%) HHF, respectively. Of all studies, n=6 (86%) and n=1 (14%) studies originated from lower-middle and upper-middle income countries, respectively and all studies (100%) were hospital-based using a prospective, single-centre design. Risk of bias was low in all studies. The estimated prevalences of mild and severe PH were 40.3% (95%CI: 21.7–60.4%; from 7 studies; Figure 1a) and 26.3% [95%CI: 9.8–47.1%] from 5 studies; Figure 1b), respectively. Decreased EF was associated with significantly increased PH prevalence estimates (p=0.032; Figure 1c).
Conclusion: PH prevalence is common in HHF and dependent on LV function. There is an urgent need for improved preventative cardiac health programs in SSA that aim at population screening and treatment of elevated BP to reduce PH burden in, and improve outcomes and quality of life of, at-risk patients.
Methods: We conducted a systematic literature search following PRISMA and GATHER guidelines searching PubMed, Embase, Web of Science, and LILACS for studies published until 09/2023 on patients in SSA with diagnosed HHF who underwent echocardiography. HHF was defined as BP>180/100mmHg, accompanied by symptoms of HF, increased LV septal thickness (>13mm), and systolic (LV ejection fraction [EF] <50%) or diastolic (EF≥50% and E/A<1) dysfunction. PH was defined as mild (tricuspid regurgitation velocity [TRV] >2.8m/s) or severe (>3.4m/s). We excluded studies without a clear PH definition and performed a meta-analysis using a random-effects model of proportions. All studies were assessed for risk of bias.
Results: We included N=7 studies, published between 2008–2019, compromising N=1,173 patients (mean age, 54±3 years; male, 53±16%). There were n=3 studies (n=371 patients) and n=4 studies (n=802) that analyzed systolic (mean EF 53±16%) and diastolic (EF 33±15%) HHF, respectively. Of all studies, n=6 (86%) and n=1 (14%) studies originated from lower-middle and upper-middle income countries, respectively and all studies (100%) were hospital-based using a prospective, single-centre design. Risk of bias was low in all studies. The estimated prevalences of mild and severe PH were 40.3% (95%CI: 21.7–60.4%; from 7 studies; Figure 1a) and 26.3% [95%CI: 9.8–47.1%] from 5 studies; Figure 1b), respectively. Decreased EF was associated with significantly increased PH prevalence estimates (p=0.032; Figure 1c).
Conclusion: PH prevalence is common in HHF and dependent on LV function. There is an urgent need for improved preventative cardiac health programs in SSA that aim at population screening and treatment of elevated BP to reduce PH burden in, and improve outcomes and quality of life of, at-risk patients.
More abstracts on this topic:
International Differences in Hemodynamic Response to Balloon Pulmonary Angioplasty in Chronic Thromboembolic Pulmonary Hypertension: A Multicenter Study from Japan and the Netherlands
Higuchi Satoshi, Lelij Rutger, Fukuda Tetsuya, Ota Hideki, De Man Frances, Post Marco, Ogo Takeshi, Vonk Noordegraaf Anton, Meijboom Lilian, Bogaard Harm, Kiko Takatoyo, Mantzios Konstantinos, Satoh Taijyu, Diederik Staal, Rodenburg Tamara, Van Kuijk Jan Peter, Boerman Sanne, Beijk M
3CPR Best Abstract Award: The pathogenic role of ADAMTS13 deficiency in Chronic Thromboembolic Pulmonary HypertensionWu Zhijian, Zheng X. Long, Zheng Liang