Final ID: Mo1030
Dissecting The Origins Of An Incidental Aortic Pseudoaneurysm
Abstract Body (Do not enter title and authors here): Background:
An aortic pseudoaneurysm (APA) is a contained rupture of the aortic wall that is often asymptomatic and detected as an incidental imaging finding. APAs can result from blunt thoracic trauma or can be iatrogenic. APAs secondary to aortic dissections are rare, and can lead to severe complications including rupture, hemorrhage, and death. Due to its high-risk nature, once discovered, prompt surgical or endovascular repair is important to prevent further complications.
Case/Methods:
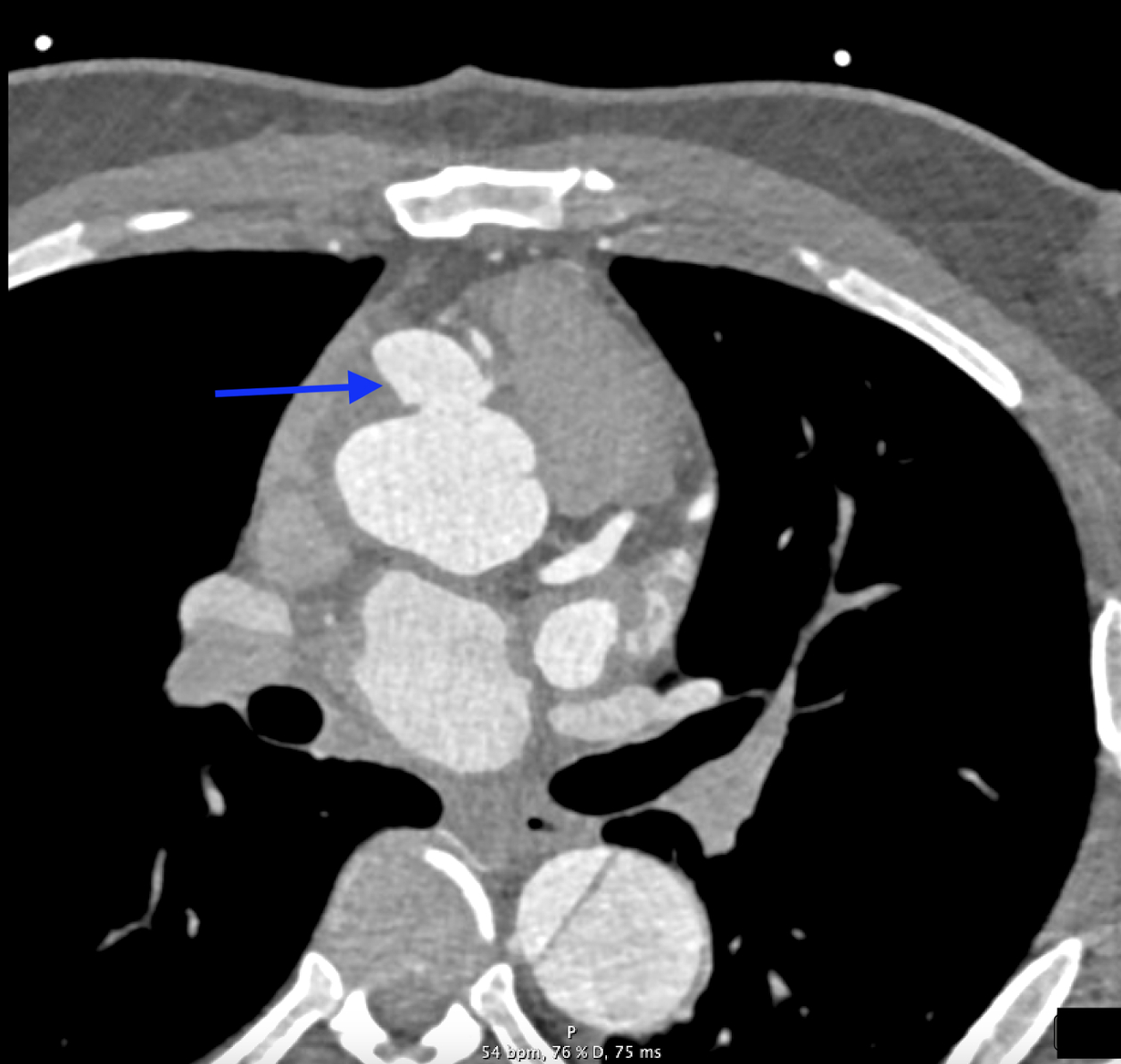
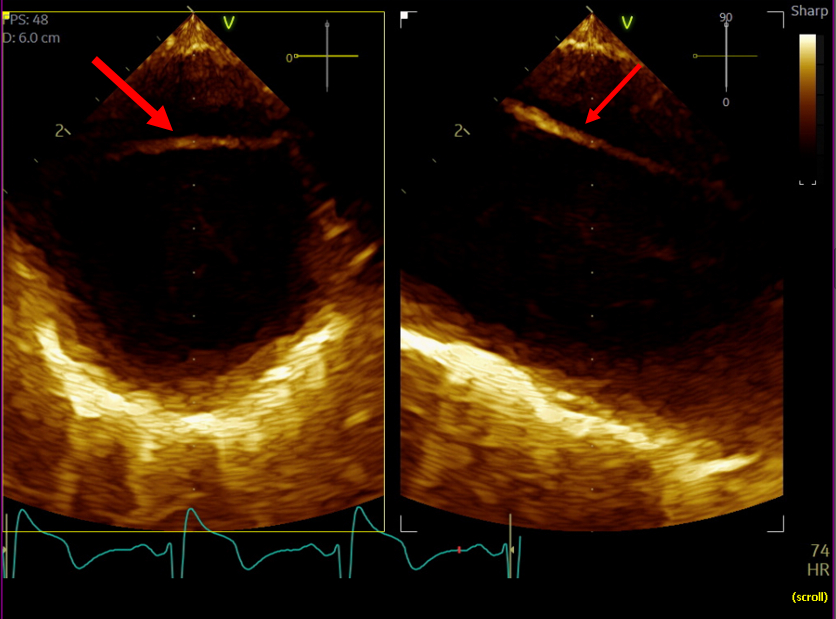
A 42-year-old male with history of a Type A aortic dissection with surgical repair 3 years earlier, resistant hypertension, hyperlipidemia, and prior tobacco use, presented for chest pain radiating to his back. Physical exam was notable for a 2/6 systolic murmur, most prominent at the aortic position. Initial vitals were significant for hypertension, with a blood pressure of 164/105 mmHg. Laboratory testing showed troponin elevated to 30 ng/L (reference < 15 ng/L), with a stable 3-hour trend. EKG showed normal sinus rhythm with left axis deviation and left ventricular hypertrophy. A CT angiography (CTA) dissection protocol showed a dissection flap distal to the left subclavian artery, extending into the abdominal aorta, consistent with a Stanford Type B aortic dissection (TBAD). The patient was managed with beta blockers and vasodilators to maintain systolic blood pressure under 120 mmHg and heart rate under 60 beats per minute. Following symptom resolution, a repeat thoracic CTA revealed a 2.5 cm sac near the origin of the right main coronary artery, representing a pseudoaneurysm not seen prior. Subsequent cardiac CTA confirmed this pseudoaneurysm outpouching secondary to degeneration of the TBAD. The patient underwent successful pseudoaneurysm repair with anastomosis construction and Dacron patch placement.
Discussion:
While the patient’s initial presentation and imaging studies, consistent with a TBAD, suggested conservative management, repeat imaging was imperative and changed the therapeutic plan despite the resolution of his symptoms. Current ACC/AHA guidelines recommend medical management for uncomplicated Type B dissections with close monitoring; however, aneurysmal progression mandates timely surgical intervention to mitigate rupture risk. This case highlights the importance of serial imaging in patients with TBADs to detect evolving complications such as APA formation, which may initially be occult but carry high mortality risk if left untreated.
An aortic pseudoaneurysm (APA) is a contained rupture of the aortic wall that is often asymptomatic and detected as an incidental imaging finding. APAs can result from blunt thoracic trauma or can be iatrogenic. APAs secondary to aortic dissections are rare, and can lead to severe complications including rupture, hemorrhage, and death. Due to its high-risk nature, once discovered, prompt surgical or endovascular repair is important to prevent further complications.
Case/Methods:
A 42-year-old male with history of a Type A aortic dissection with surgical repair 3 years earlier, resistant hypertension, hyperlipidemia, and prior tobacco use, presented for chest pain radiating to his back. Physical exam was notable for a 2/6 systolic murmur, most prominent at the aortic position. Initial vitals were significant for hypertension, with a blood pressure of 164/105 mmHg. Laboratory testing showed troponin elevated to 30 ng/L (reference < 15 ng/L), with a stable 3-hour trend. EKG showed normal sinus rhythm with left axis deviation and left ventricular hypertrophy. A CT angiography (CTA) dissection protocol showed a dissection flap distal to the left subclavian artery, extending into the abdominal aorta, consistent with a Stanford Type B aortic dissection (TBAD). The patient was managed with beta blockers and vasodilators to maintain systolic blood pressure under 120 mmHg and heart rate under 60 beats per minute. Following symptom resolution, a repeat thoracic CTA revealed a 2.5 cm sac near the origin of the right main coronary artery, representing a pseudoaneurysm not seen prior. Subsequent cardiac CTA confirmed this pseudoaneurysm outpouching secondary to degeneration of the TBAD. The patient underwent successful pseudoaneurysm repair with anastomosis construction and Dacron patch placement.
Discussion:
While the patient’s initial presentation and imaging studies, consistent with a TBAD, suggested conservative management, repeat imaging was imperative and changed the therapeutic plan despite the resolution of his symptoms. Current ACC/AHA guidelines recommend medical management for uncomplicated Type B dissections with close monitoring; however, aneurysmal progression mandates timely surgical intervention to mitigate rupture risk. This case highlights the importance of serial imaging in patients with TBADs to detect evolving complications such as APA formation, which may initially be occult but carry high mortality risk if left untreated.
More abstracts on this topic:
Aortic Root Pseudoaneurysm Following Bicuspid Aortic Valve Endocarditis and Root Reconstruction
Odai Reuben, Kutilek Frank, Alchaer Anthony, Sajjad Laiba, Farhoud Hussam
84 Immune checkpoint profiling in major aortic diseases leads to identification of potential roles of CD155-CD206 pathway in suppressing inflammation and immune responsesShao Ying, Saaoud Fatma, Xu Keman, Lu Yifan, Jiang Xiaohua, Wang Hong, Yang Xiaofeng