Final ID: MP41
High-output Heart Failure in Acute Respiratory Distress Syndrome: A Secondary Analysis of the FACTT Trial
Abstract Body (Do not enter title and authors here): Introduction: Acute respiratory distress syndrome (ARDS) is characterized by pulmonary edema, hypoxia and systemic inflammation. The presence and clinical implications of a high cardiac output state in patients with ARDS remain unknown given the lack of invasive hemodynamic monitoring in most patients with ARDS.
Hypothesis: A subset of patients with ARDS will have high output heart failure with high cardiac output and elevated pulmonary capillary wedge pressure (PAWP) representing a unique subphenotype of ARDS.
Methods: Patients from the Comparison of Two Fluid-Management Strategies in Acute Lung Injury (FACTT) Trial were stratified according to baseline cardiac output states and filling pressures: HOLHF (high-output with left heart failure) was defined as cardiac index (CI) ≥ 4 L/min/m2 and PAWP ≥ 15 mmHg; HOnoLHF (high-output without left heart failure) as CI ≥ 4 L/min/m2 and PAWP < 15 mmHg; and NOHO (non-high-output) as CI < 4 L/min/m2. Hemodynamics, oxygenation, metabolic demand (VO2) and clinical outcomes were compared across groups.
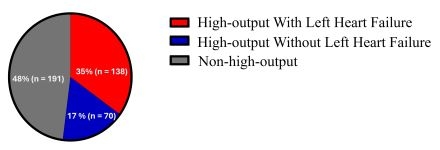
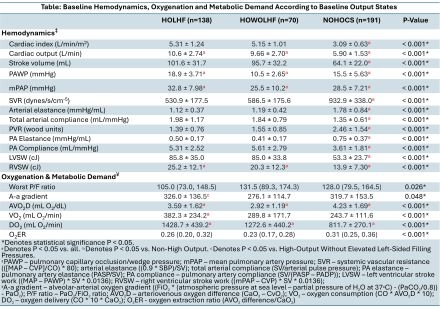
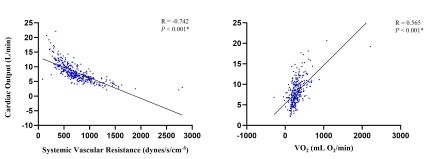
Results: Of the 399 patients included, high-output states were present in 52% of all patients (Figure 1). High-output cohorts demonstrated higher myocardial workload, lower systemic vascular resistance (SVR), lower pulsatile arterial load, higher VO2 and more impaired systemic O2 utilization despite the highest peripheral O2 delivery compared to NOHO (Table). Among the high-output cohorts, the HOLHF cohort demonstrated higher right ventricular stroke work (25.2 ± 12.1 vs. 20.3 ± 12.3, P<0.001), worse A-a gradient (326.0 ± 136.5 vs. 276.1 ± 114.7, P=0.048) and higher VO2 (382.3 ± 234.2 vs. 289.8 ± 171.7, P<0.001) compared to HOnoLHF. Increasing cardiac output was individually related to decreasing SVR (r=-0.742, P<0.001) and increasing VO2 (r=0.565, P<0.001) (Figure 2). When adjusted, both variables remained strongly related to increasing cardiac output (P<0.001). There were no significant differences among the cohorts with respect to refractory hypoxia and mortality.
Conclusions: High-output states in ARDS are prevalent and underrecognized. Such states appear to be driven by arterial vasodilatation and heightened VO2 with additional manifestations of increased myocardial workload and inefficient peripheral utilization with impaired systemic O2 utilization. Whether specific strategies to mitigate the high output state might improve gas exchange, hypoxia and outcomes in patients with HOLHF and ARDS requires further study.
Hypothesis: A subset of patients with ARDS will have high output heart failure with high cardiac output and elevated pulmonary capillary wedge pressure (PAWP) representing a unique subphenotype of ARDS.
Methods: Patients from the Comparison of Two Fluid-Management Strategies in Acute Lung Injury (FACTT) Trial were stratified according to baseline cardiac output states and filling pressures: HOLHF (high-output with left heart failure) was defined as cardiac index (CI) ≥ 4 L/min/m2 and PAWP ≥ 15 mmHg; HOnoLHF (high-output without left heart failure) as CI ≥ 4 L/min/m2 and PAWP < 15 mmHg; and NOHO (non-high-output) as CI < 4 L/min/m2. Hemodynamics, oxygenation, metabolic demand (VO2) and clinical outcomes were compared across groups.
Results: Of the 399 patients included, high-output states were present in 52% of all patients (Figure 1). High-output cohorts demonstrated higher myocardial workload, lower systemic vascular resistance (SVR), lower pulsatile arterial load, higher VO2 and more impaired systemic O2 utilization despite the highest peripheral O2 delivery compared to NOHO (Table). Among the high-output cohorts, the HOLHF cohort demonstrated higher right ventricular stroke work (25.2 ± 12.1 vs. 20.3 ± 12.3, P<0.001), worse A-a gradient (326.0 ± 136.5 vs. 276.1 ± 114.7, P=0.048) and higher VO2 (382.3 ± 234.2 vs. 289.8 ± 171.7, P<0.001) compared to HOnoLHF. Increasing cardiac output was individually related to decreasing SVR (r=-0.742, P<0.001) and increasing VO2 (r=0.565, P<0.001) (Figure 2). When adjusted, both variables remained strongly related to increasing cardiac output (P<0.001). There were no significant differences among the cohorts with respect to refractory hypoxia and mortality.
Conclusions: High-output states in ARDS are prevalent and underrecognized. Such states appear to be driven by arterial vasodilatation and heightened VO2 with additional manifestations of increased myocardial workload and inefficient peripheral utilization with impaired systemic O2 utilization. Whether specific strategies to mitigate the high output state might improve gas exchange, hypoxia and outcomes in patients with HOLHF and ARDS requires further study.
More abstracts on this topic:
A Comparison of Anxiety and Depression in Patients with Symptoms of Palpitations Compared to High Risk Arrythmia Patients.
Treuth Mark, Patel Kunnal, Rissmiller Justin, Holdai Veera
A Remote Patient Care Heart Failure Program Drives Improved Clinical Outcomes and Reduced Healthcare Cost and UtilizationFeldman David, Reynolds Spencer, Curnow Randall, Cunningham Eve, Feldman Theodore, Fudim Marat