Final ID: Mo3125
Successful Management of Acute Ischemic Stroke in the Context of Chronic Stanford Type A/DeBakey Type I Aortic Dissection: A Multidisciplinary Approach with Mechanical Thrombectomy via Direct Carotid Artery Access
Abstract Body (Do not enter title and authors here): Introduction: Acute ischemic stroke is a known complication of aortic dissection (AD), either by extension, thromboembolism, or cerebral hypoperfusion. The incidence ranges from 6–32% among patients with AD.
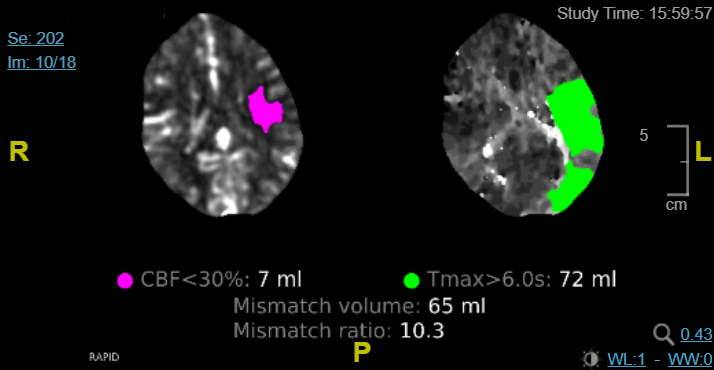
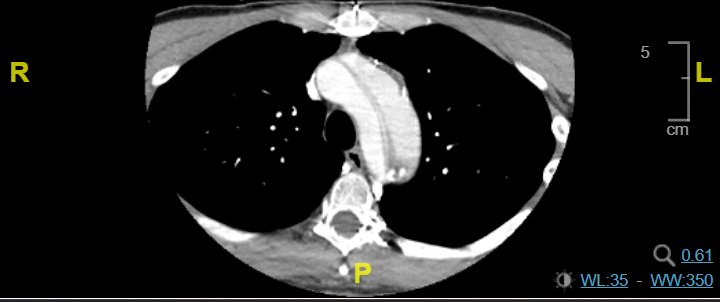
Case Presentation: A 42-year-old male with a history of hypertension and chronic Stanford type A/DeBakey I AD post aortic arch and valve repair (11 years prior), with thoracoabdominal dissection and aneurysmal changes, presented with difficulty in speech and unsteady gait. Blood pressure (BP) was 183/102 mmHg. ECG showed normal sinus rhythm. The last well-known was 45 minutes before the presentation; the National Institutes of Health stroke scale (NIHSS) was 6. The non-contrast CT head was unremarkable; CT angio showed left M2 MCA occlusion in the Sylvian fissure, Stanford type A AD with flaps crossing the origins of the brachiocephalic, left common carotid, and left subclavian. CT head perfusion revealed 65 cc of ischemic penumbra in the left MCA territory and a core infarct of 7 cc. MRI of the brain revealed an acute infarct in the left frontal and parietal lobes; CT chest/abdomen/pelvis showed an aneurysmal thoracoabdominal aorta (descending: 6x5.9 cm; suprarenal: 4.1x4 cm; infrarenal: 5.4x6.1 cm) with mural thrombus in the false lumen. On day 0, his mental status declined, NIHSS increased to 16 and he required intubation. He was taken for emergent percutaneous intracranial mechanical thrombectomy (MT) through left carotid artery access by vascular surgery, followed by interventional neurology rescue and achieved thrombolysis in cerebral ischemia score (TICI) 2C. He was extubated on day 1, and NIHSS improved to 3 over the next 3 days.
Discussion: In our patient, chronic AD with mural thrombus, chronic tobacco use, hypertension, and dyslipidemia increased the risk of stroke. Intravenous thrombolysis among patients with AD can lead to serious complications, including aortic rupture and cardiac tamponade. MT may improve neurologic outcomes. AIS secondary to large vessel occlusion in our patient led to worsening neurological function, which was significantly improved after MT with near-complete reperfusion. In our patient, carotid access was chosen as femoral access poses a high risk in AD. MT is a standard intervention secondary to large vessel occlusion, but data regarding the efficacy of MT among patients with AD is sparse. He was discharged on apixaban; antihypertensives were optimized, and cardiology follow-up was arranged for elective aortic repair.
Case Presentation: A 42-year-old male with a history of hypertension and chronic Stanford type A/DeBakey I AD post aortic arch and valve repair (11 years prior), with thoracoabdominal dissection and aneurysmal changes, presented with difficulty in speech and unsteady gait. Blood pressure (BP) was 183/102 mmHg. ECG showed normal sinus rhythm. The last well-known was 45 minutes before the presentation; the National Institutes of Health stroke scale (NIHSS) was 6. The non-contrast CT head was unremarkable; CT angio showed left M2 MCA occlusion in the Sylvian fissure, Stanford type A AD with flaps crossing the origins of the brachiocephalic, left common carotid, and left subclavian. CT head perfusion revealed 65 cc of ischemic penumbra in the left MCA territory and a core infarct of 7 cc. MRI of the brain revealed an acute infarct in the left frontal and parietal lobes; CT chest/abdomen/pelvis showed an aneurysmal thoracoabdominal aorta (descending: 6x5.9 cm; suprarenal: 4.1x4 cm; infrarenal: 5.4x6.1 cm) with mural thrombus in the false lumen. On day 0, his mental status declined, NIHSS increased to 16 and he required intubation. He was taken for emergent percutaneous intracranial mechanical thrombectomy (MT) through left carotid artery access by vascular surgery, followed by interventional neurology rescue and achieved thrombolysis in cerebral ischemia score (TICI) 2C. He was extubated on day 1, and NIHSS improved to 3 over the next 3 days.
Discussion: In our patient, chronic AD with mural thrombus, chronic tobacco use, hypertension, and dyslipidemia increased the risk of stroke. Intravenous thrombolysis among patients with AD can lead to serious complications, including aortic rupture and cardiac tamponade. MT may improve neurologic outcomes. AIS secondary to large vessel occlusion in our patient led to worsening neurological function, which was significantly improved after MT with near-complete reperfusion. In our patient, carotid access was chosen as femoral access poses a high risk in AD. MT is a standard intervention secondary to large vessel occlusion, but data regarding the efficacy of MT among patients with AD is sparse. He was discharged on apixaban; antihypertensives were optimized, and cardiology follow-up was arranged for elective aortic repair.
More abstracts on this topic:
Aortic Growth Mapping to Examine Genotype-Phenotype Correlations in Heritable Thoracic Aortic Disease and Variants of Unknown Significance
Campello Carlos Alberto, Ramesh Vedika, Marway Prabhvir, Hofmann Bowman Marion, Aatre Rajani, Burris Nicholas
Ascending Thoracic Aortic Aneurysms in a Veterans Affairs Health System: Longitudinal Outcomes and Risk FactorsGomez Axel, Carroway William, Ge Liang, Boskovski Marko, Tseng Elaine