Final ID: EPI20
Incident venous thromboembolism and subsequent risk of cardiovascular outcomes: the Atherosclerosis Risk in Communities (ARIC) study
Abstract Body (Do not enter title and authors here): Background: Venous thromboembolism (VTE) and atherothrombosis have different mechanisms of thrombosis formation. A few previous studies reported those having a VTE have greater risk of incident atherothrombotic disease. These studies have several limitations, such as inadequate adjustment for key confounders (e.g., obesity), selected study populations in clinical trials, and small sample size. Moreover, the links of VTE to heart failure (HF) and peripheral artery disease (PAD) are not well understood.
Hypothesis: VTE is independently associated with a range of incident cardiovascular outcomes.
Methods: In 12,988 ARIC participants without history of VTE or cardiovascular disease at baseline (1987-89), we quantified the association of VTE, as a time-varying exposure, with incident myocardial infarction (MI), stroke, HF, PAD (overall and its severe form, critical limb ischemia [CLI]) using multivariable Cox regression. We also considered unprovoked and provoked VTE separately.
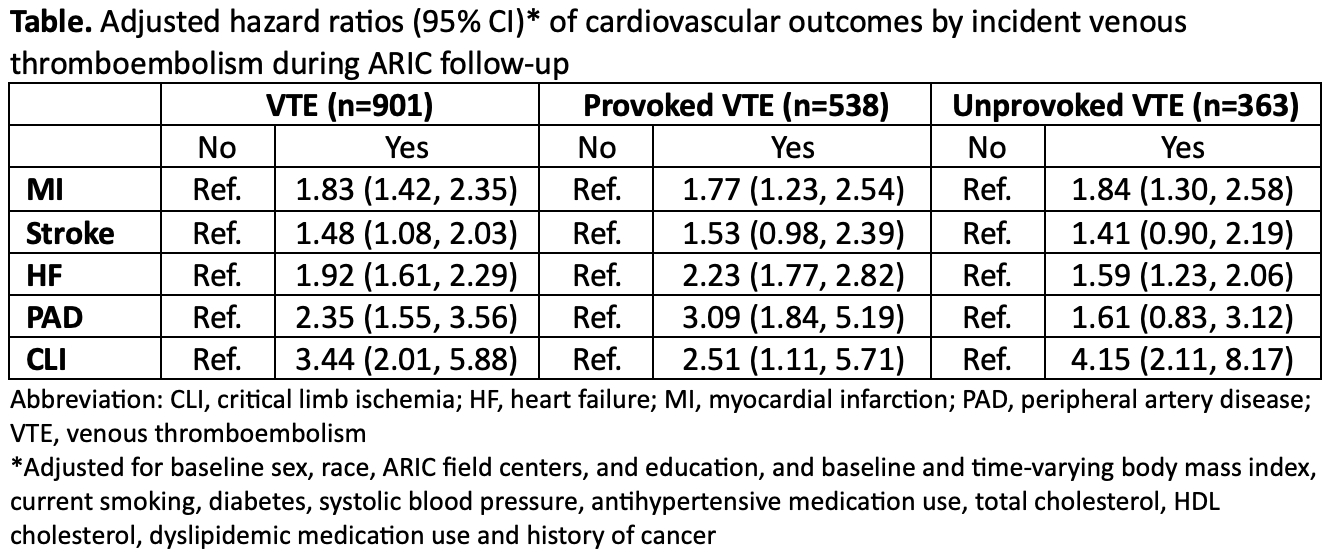
Results: Over a median follow-up of 25 years, 901 participants experienced incident VTE. In the same timeframe, there were 1,950 MI events, 1,247 stroke events, 2,981 HF events, and 516 PAD cases (including 207 CLI cases). Participants with VTE, compared to those without, had a higher risk of all cardiovascular outcomes (Table). The associations were particularly evident for incident PAD and CLI (adjusted HR 2.32 [95% CI 1.53, 3.52] and 3.44 [2.01, 5.88], respectively). Provoked VTE showed similar associations with all cardiovascular outcomes, whereas unprovoked VTE was significantly associated with MI, HF, and CLI only (Table).
Conclusions: In this large community-based study, VTE was robustly associated with subsequent risk of different cardiovascular outcomes, independent of potential confounders. Patients with VTE should be considered at high risk of other cardiovascular outcomes and receive optimal preventive therapy for cardiovascular diseases, including atherosclerotic disease and HF.
Hypothesis: VTE is independently associated with a range of incident cardiovascular outcomes.
Methods: In 12,988 ARIC participants without history of VTE or cardiovascular disease at baseline (1987-89), we quantified the association of VTE, as a time-varying exposure, with incident myocardial infarction (MI), stroke, HF, PAD (overall and its severe form, critical limb ischemia [CLI]) using multivariable Cox regression. We also considered unprovoked and provoked VTE separately.
Results: Over a median follow-up of 25 years, 901 participants experienced incident VTE. In the same timeframe, there were 1,950 MI events, 1,247 stroke events, 2,981 HF events, and 516 PAD cases (including 207 CLI cases). Participants with VTE, compared to those without, had a higher risk of all cardiovascular outcomes (Table). The associations were particularly evident for incident PAD and CLI (adjusted HR 2.32 [95% CI 1.53, 3.52] and 3.44 [2.01, 5.88], respectively). Provoked VTE showed similar associations with all cardiovascular outcomes, whereas unprovoked VTE was significantly associated with MI, HF, and CLI only (Table).
Conclusions: In this large community-based study, VTE was robustly associated with subsequent risk of different cardiovascular outcomes, independent of potential confounders. Patients with VTE should be considered at high risk of other cardiovascular outcomes and receive optimal preventive therapy for cardiovascular diseases, including atherosclerotic disease and HF.
More abstracts on this topic:
3-Minute Heart Health App: A Feasibility Study
Abdulkarim Iya, Metzger Joseph, Stovitz Steven, Van't Hof Jeremy
A Novel Animal Model for Pulmonary Hypertension: Lung Endothelial Specific Deletion of Egln1 in MiceLiu Bin, Yi Dan, Ramirez Karina, Fallon Michael, Dai Zhiyu