Final ID: EPI11
Actigraphy-Measured Sleep Irregularity Increases the Risk of Incident Cardiovascular Disease and Cardiovascular Mortality in Older Women
Abstract Body (Do not enter title and authors here): Background: Cardiovascular disease (CVD) is the leading cause of death for U.S. women. Our understanding of the link between poor sleep health and CVD remains limited by reliance on cross-sectional study designs, self-reported sleep measures, and predominately non-Hispanic white participants. Our objective was to investigate associations between actigraphy-measured sleep health and incident CVD and CVD mortality in a cohort of older multiethnic women.
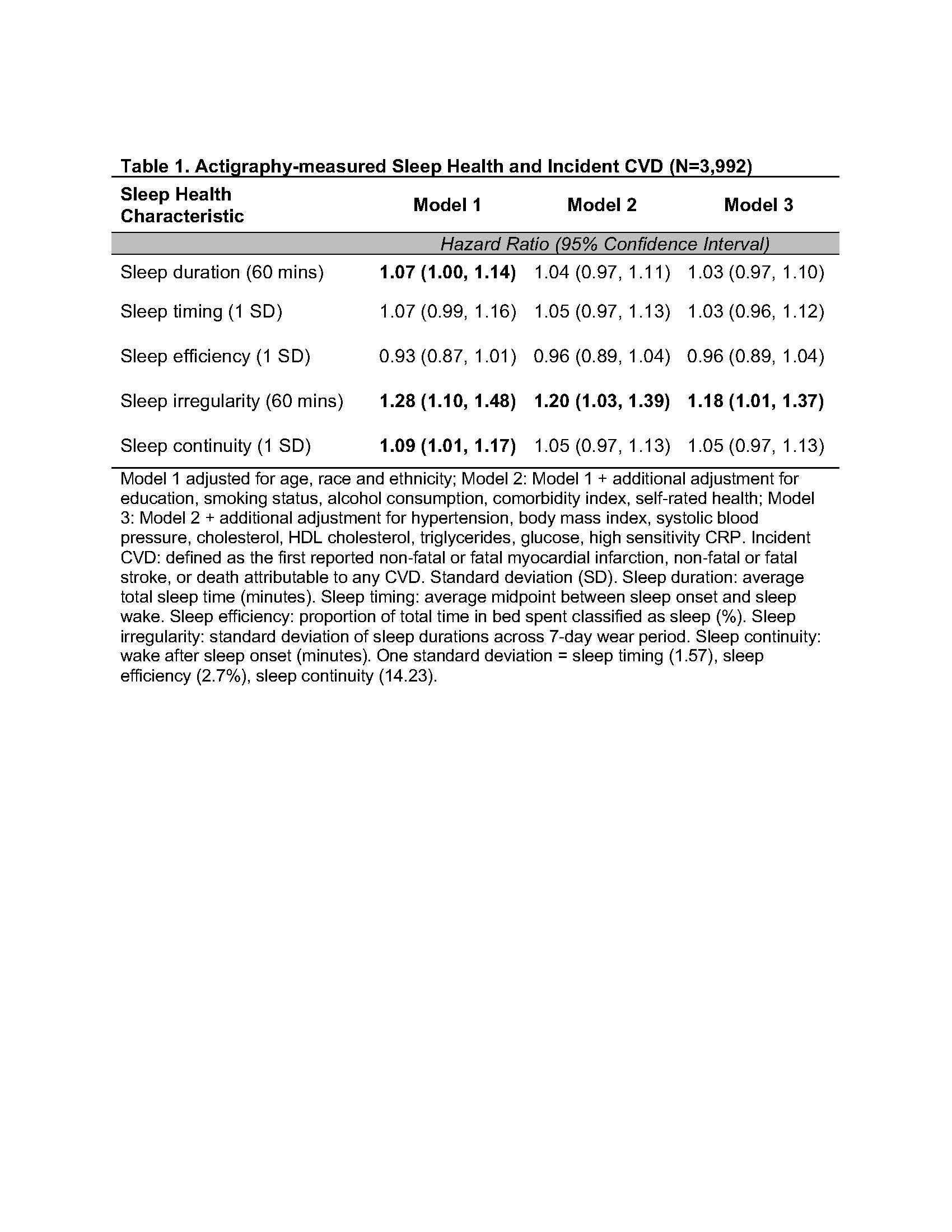
Methods: Women (n=3,992; mean age: 78.5 years, 33% African American, 17% Hispanic/Latino) enrolled in the Women’s Health Initiative OPACH (Objective Physical Activity and Cardiovascular Health) study wore an Actigraph GT3X+ accelerometer for 7 days in May 2012-April 2014 and were followed through February 2022 for physician-adjudicated incident CVD (myocardial infarction, stroke, or death due to CVD) and CVD mortality. Sleep duration, timing, efficiency, irregularity, and continuity were derived from accelerometers (see Table footnote). Women with a history of prior CVD at the time of accelerometer wear were excluded. We used Cox proportional hazards regression to estimate hazard ratios (HRs) and 95% confidence intervals (CIs). Minimally adjusted models included age, race, and ethnicity. Models were additionally adjusted for education, smoking status, alcohol use, comorbid conditions, self-rated health, and CVD risk factors including hypertension, body mass index, systolic blood pressure, cholesterol, and glucose.
Results: Over a median of 8.3 years of follow-up, 636 incident CVD cases occurred, including 395 CVD deaths. In minimally adjusted models, longer sleep duration, greater sleep irregularity, and more wake after sleep onset were associated with increased CVD risk (Table 1). In models further adjusted for CVD risk factors, the HR (95% CI) for a 60-minute increase in sleep irregularity was 1.18 (1.01-1.37) for incident CVD and 1.30 (1.07-1.58) for CVD mortality.
Conclusions: Greater sleep irregularity was associated with higher risk of incident CVD and CVD mortality in a cohort of older women. These results support the importance of maintaining regular sleep for cardiovascular health.
Methods: Women (n=3,992; mean age: 78.5 years, 33% African American, 17% Hispanic/Latino) enrolled in the Women’s Health Initiative OPACH (Objective Physical Activity and Cardiovascular Health) study wore an Actigraph GT3X+ accelerometer for 7 days in May 2012-April 2014 and were followed through February 2022 for physician-adjudicated incident CVD (myocardial infarction, stroke, or death due to CVD) and CVD mortality. Sleep duration, timing, efficiency, irregularity, and continuity were derived from accelerometers (see Table footnote). Women with a history of prior CVD at the time of accelerometer wear were excluded. We used Cox proportional hazards regression to estimate hazard ratios (HRs) and 95% confidence intervals (CIs). Minimally adjusted models included age, race, and ethnicity. Models were additionally adjusted for education, smoking status, alcohol use, comorbid conditions, self-rated health, and CVD risk factors including hypertension, body mass index, systolic blood pressure, cholesterol, and glucose.
Results: Over a median of 8.3 years of follow-up, 636 incident CVD cases occurred, including 395 CVD deaths. In minimally adjusted models, longer sleep duration, greater sleep irregularity, and more wake after sleep onset were associated with increased CVD risk (Table 1). In models further adjusted for CVD risk factors, the HR (95% CI) for a 60-minute increase in sleep irregularity was 1.18 (1.01-1.37) for incident CVD and 1.30 (1.07-1.58) for CVD mortality.
Conclusions: Greater sleep irregularity was associated with higher risk of incident CVD and CVD mortality in a cohort of older women. These results support the importance of maintaining regular sleep for cardiovascular health.
More abstracts on this topic:
Beyond the Beat: Mobile Health Technology Reveals Hidden Sleep-Activity-Mood Connections in Community-Dwelling Heart Failure Patients
Huang Tsuey-yuan, Tsai Ming-fen, Moser Debra
Association Of Sleep Irregularity And Variability With Leptin And Adiponectin Levels In AdolescentsBallester-navarro Pura, Morales-ghinaglia Natasha, Lenker Kristina, Calhoun Susan, Liao Jiangang, Vgontzas Alexandros, Liao Duanping, Bixler Edward, Fernandez-mendoza Julio