Final ID: Mo1030
Trends in Critical Limb Ischaemia Related Mortality in Patients Aged 55 and Older in the United States: Insights from the CDC WONDER Database
Abstract Body (Do not enter title and authors here): Background: Critical Limb Ischaemia (CLI) is a concerning medical emergency condition with notable mortality among older adults. This study highlights the trends and demographic disparities in mortality rates due to CLI in patients aged 55 and older in the United States from 1999 to 2020.
Aim: This study aimed to evaluate patterns and geographical variations in mortality associated with CLI among adults in the United States.
Methods: Death certificates from CDC WONDER database from1999 to 2020 were analyzed to investigate mortality related to CLI among adults. Age-adjusted mortality rates (AAMRs) per 100,000 persons were calculated, stratified by year, sex, race/ethnicity, and geographical regions.
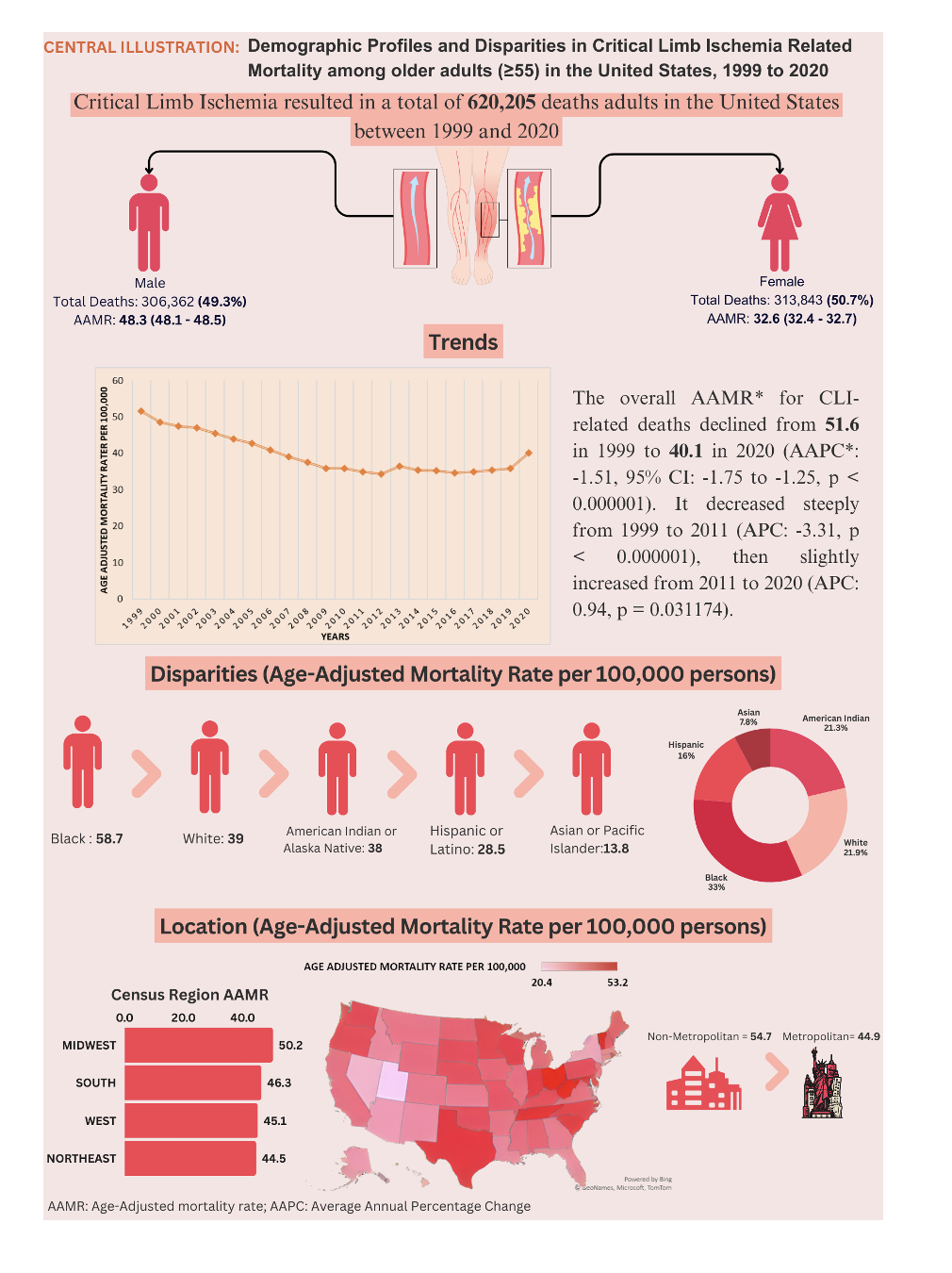
Results: CLI caused a concerning 620,205 deaths among US adults aged 55+ between 1999 and 2020, primarily in hospitals (42%). The overall AAMR for CLI-related deaths showed decline from 51.6 in 1999 to 40.1 in 2020, with an AAPC of -1.51 (95% CI: -1.75 to -1.25, p < 0.000001). The AAMR experienced a steeper decrease from 1999 to 2011 (APC: -3.31, p < 0.000001), followed by a slight increase from 2011 to 2020 (APC: 0.94, p = 0.031174). Men had higher AAMRs than women, though both sexes experienced reductions (men: 48.3; women: 32.6). The AAMR for men decreased from 64.9 in 1999 to 42.8 in 2011, increasing to 50.1 by 2020. For women, the AAMR decreased from 42.9 in 1999 to 28.3 in 2014, followed by a slight increase to 32.3 by 2020. Racial/ethnic disparities were apparent, with Black individuals having the highest AAMRs (58.7), followed by Whites (39.0), American Indians/Alaska Natives (38.0), Hispanics (28.5), and Asians/Pacific Islanders (13.8). All racial groups experienced decreases in AAMRs. Geographically, AAMRs varied from 20.4 in Utah to 53.2 in Ohio. The highest mortality noted in the Midwestern region (AAMR: 43). Nonmetropolitan areas unveiled higher AAMRs than metropolitan areas (nonmetropolitan: 43.5; metropolitan: 38.2). Both regions showed a decrease in AAMRs from 1999 to 2020 (metropolitan AAPC: -1.36, p < 0.000001; nonmetropolitan AAPC: -0.81, p = 0.001399).
Conclusion: Our analysis highlights significant demographic and geographic differences in older adult mortality due to CLI in the U.S. Continued decreases over time but recent upturn in mortality rates emphasizes need for focused interventions to close these gaps and to improve population health outcomes for affected populations.
Aim: This study aimed to evaluate patterns and geographical variations in mortality associated with CLI among adults in the United States.
Methods: Death certificates from CDC WONDER database from1999 to 2020 were analyzed to investigate mortality related to CLI among adults. Age-adjusted mortality rates (AAMRs) per 100,000 persons were calculated, stratified by year, sex, race/ethnicity, and geographical regions.
Results: CLI caused a concerning 620,205 deaths among US adults aged 55+ between 1999 and 2020, primarily in hospitals (42%). The overall AAMR for CLI-related deaths showed decline from 51.6 in 1999 to 40.1 in 2020, with an AAPC of -1.51 (95% CI: -1.75 to -1.25, p < 0.000001). The AAMR experienced a steeper decrease from 1999 to 2011 (APC: -3.31, p < 0.000001), followed by a slight increase from 2011 to 2020 (APC: 0.94, p = 0.031174). Men had higher AAMRs than women, though both sexes experienced reductions (men: 48.3; women: 32.6). The AAMR for men decreased from 64.9 in 1999 to 42.8 in 2011, increasing to 50.1 by 2020. For women, the AAMR decreased from 42.9 in 1999 to 28.3 in 2014, followed by a slight increase to 32.3 by 2020. Racial/ethnic disparities were apparent, with Black individuals having the highest AAMRs (58.7), followed by Whites (39.0), American Indians/Alaska Natives (38.0), Hispanics (28.5), and Asians/Pacific Islanders (13.8). All racial groups experienced decreases in AAMRs. Geographically, AAMRs varied from 20.4 in Utah to 53.2 in Ohio. The highest mortality noted in the Midwestern region (AAMR: 43). Nonmetropolitan areas unveiled higher AAMRs than metropolitan areas (nonmetropolitan: 43.5; metropolitan: 38.2). Both regions showed a decrease in AAMRs from 1999 to 2020 (metropolitan AAPC: -1.36, p < 0.000001; nonmetropolitan AAPC: -0.81, p = 0.001399).
Conclusion: Our analysis highlights significant demographic and geographic differences in older adult mortality due to CLI in the U.S. Continued decreases over time but recent upturn in mortality rates emphasizes need for focused interventions to close these gaps and to improve population health outcomes for affected populations.
More abstracts on this topic:
A Meta-analysis of Folic Acid Supplementation Efficacy in Cardiovascular Diseases Prevention.
Calderon Martinez Ernesto, Camacho Davila Karen Fabiola, Pinto-colmenarez Rafael, Arruarana Victor, Arvelaez Pascucci Joanne, Castillo Jaqueline Livier, Alonso Ramirez Angie Carolina, Ghattas Patricia, Giron De Marza Maria, Sosaya Zuñiga Briggitte Solange, Martinez Lilan Jonathan David, Paredes Romero Enrique
A Contemporary Machine Learning-Based Risk Stratification for Mortality and Hospitalization in Heart Failure with Preserved Ejection Fraction Using Multimodal Real-World DataFudim Marat, Weerts Jerremy, Patel Manesh, Balu Suresh, Hintze Bradley, Torres Francisco, Micsinai Balan Mariann, Rigolli Marzia, Kessler Paul, Touzot Maxime, Lund Lars, Van Empel Vanessa, Pradhan Aruna, Butler Javed, Zehnder Tobias, Sauty Benoit, Esposito Christian, Balazard Félix, Mayer Imke, Hallal Mohammad, Loiseau Nicolas