Final ID: MDP176
Comparative Analysis of the 30-Year Survival after Primary Transplant Versus Reconstructive Surgery for Hypoplastic Left Heart Syndrome
Abstract Body (Do not enter title and authors here): Background: Reconstructive surgery for hypoplastic left heart syndrome (HLHS) starts with the Norwood procedure in early infancy. Primary transplant is an alternative strategy that has shown superior outcomes to reconstructive surgery in some patients with left heart obstructive lesions. This study compares the 30-year survival of HLHS following primary transplant vs. reconstructive surgery.
Methods: Using data from the Pediatric Cardiac Care Consortium (PCCC), a large US-based registry for congenital heart surgeries, we included patients operated at <6 mos old performing both Norwood and primary transplant for HLHS between 1987 and 2003. Deaths were tracked through 2022 by the US National Death Index. Kaplan-Meier curves and extended Cox regression models were used for survival comparison after adjusting for sex, race and birth era. We also performed subgroup analysis by birth era (early: 1987-1996 vs. late: 1997-2003).
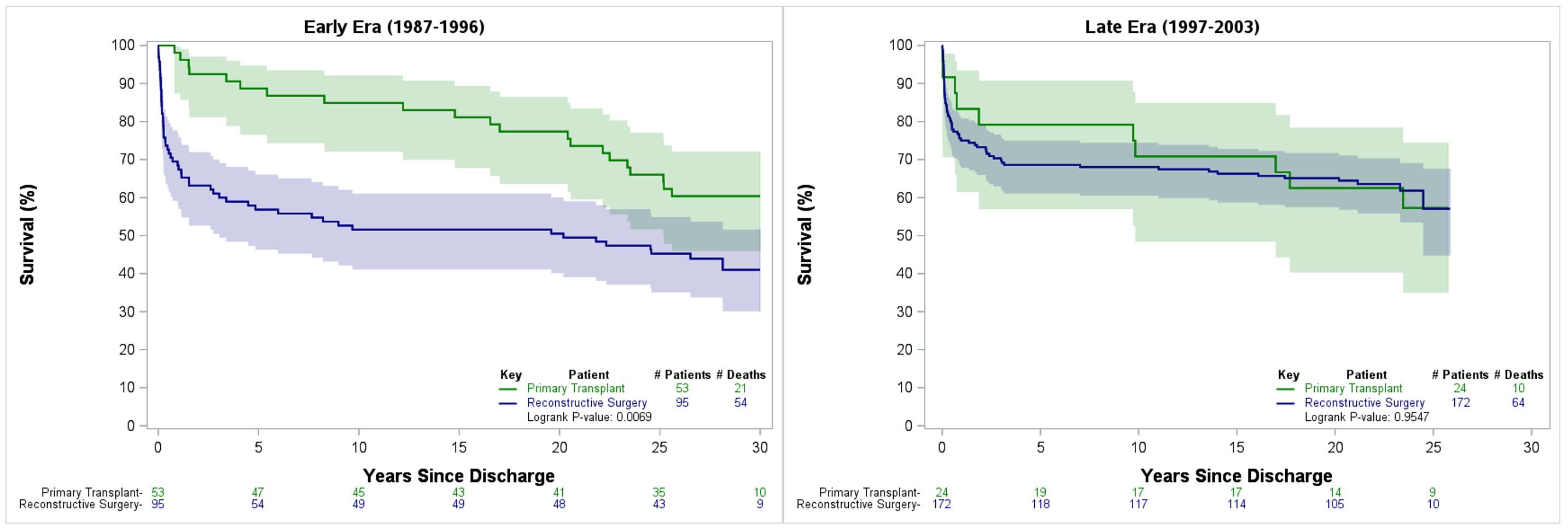
Results: Of 573 patients (males 61%) from 13 PCCC centers, 97 (17%) had a primary transplant. Patients with reconstructive surgery were younger at operation, less likely to be White, and more likely born in the late era. In-hospital survival was higher for primary transplant (79 % vs. 56%, p<0.01) with the advantage remaining significant after adjustment (aOR 0.36; 95%CI: 0.21-0.62, p<0.01). Over a median follow-up of 21.1 years (IQR 1.5, 25.3), 149 deaths occurred post-discharge. No significant difference was found between primary transplant vs. reconstructive surgery in the 30-year post-discharge survival (58.6% vs. 48.7%, p=0.07), although there was a trend towards significance after adjustment (aHR 0.68, 95% CI 0.45-1.05, p=0.08). During early era, primary transplant had 60% decreased hazard of death (aHR 0.40, 95%CI 0.23-0.72, p<0.01) compared to reconstructive surgery, while no difference was found in the late era (aHR 0.99, 95% CI 0.50-1.97, p=0.98) (Figure).
Conclusion: Primary transplant for HLHS was associated with improved 30-year survival. However, this improvement reached significance only in the early era suggesting improved outcomes with reconstructive procedures in recent years. Further analysis beyond survival is needed to elucidate the relative outcomes of these two strategies.
Methods: Using data from the Pediatric Cardiac Care Consortium (PCCC), a large US-based registry for congenital heart surgeries, we included patients operated at <6 mos old performing both Norwood and primary transplant for HLHS between 1987 and 2003. Deaths were tracked through 2022 by the US National Death Index. Kaplan-Meier curves and extended Cox regression models were used for survival comparison after adjusting for sex, race and birth era. We also performed subgroup analysis by birth era (early: 1987-1996 vs. late: 1997-2003).
Results: Of 573 patients (males 61%) from 13 PCCC centers, 97 (17%) had a primary transplant. Patients with reconstructive surgery were younger at operation, less likely to be White, and more likely born in the late era. In-hospital survival was higher for primary transplant (79 % vs. 56%, p<0.01) with the advantage remaining significant after adjustment (aOR 0.36; 95%CI: 0.21-0.62, p<0.01). Over a median follow-up of 21.1 years (IQR 1.5, 25.3), 149 deaths occurred post-discharge. No significant difference was found between primary transplant vs. reconstructive surgery in the 30-year post-discharge survival (58.6% vs. 48.7%, p=0.07), although there was a trend towards significance after adjustment (aHR 0.68, 95% CI 0.45-1.05, p=0.08). During early era, primary transplant had 60% decreased hazard of death (aHR 0.40, 95%CI 0.23-0.72, p<0.01) compared to reconstructive surgery, while no difference was found in the late era (aHR 0.99, 95% CI 0.50-1.97, p=0.98) (Figure).
Conclusion: Primary transplant for HLHS was associated with improved 30-year survival. However, this improvement reached significance only in the early era suggesting improved outcomes with reconstructive procedures in recent years. Further analysis beyond survival is needed to elucidate the relative outcomes of these two strategies.
More abstracts on this topic:
A novel small molecule synthesized based on a snail hibernation model induces hibernation in mouse fibroblasts and perfused hearts
Piao Jiyuan, Zhang Yongneng, Zhao Yuan Yuan, Hannington Patrick, Tabatabaei Dakhili Seyed Amirhossein, Ussher John, Sutendra Gopinath, Michelakis Evangelos
Abnormal Liver Stiffness as a Risk Factor for Elevated Hemoglobin A1c in Patients with Fontan PhysiologyTumuluru Priya, Lockhart Elli, Carr Michael, Kriegermeier Alyssa, Laternser Christina, Patel Sheetal