Final ID: Sa3172
Missed Opportunities To Optimize Lipid-lowering Therapy Following Revascularization In Patients With ASCVD
Research Questions: Following revascularization for ASCVD, how often do clinicians have the opportunity to obtain follow-up lipid profiles and intensify LLT?
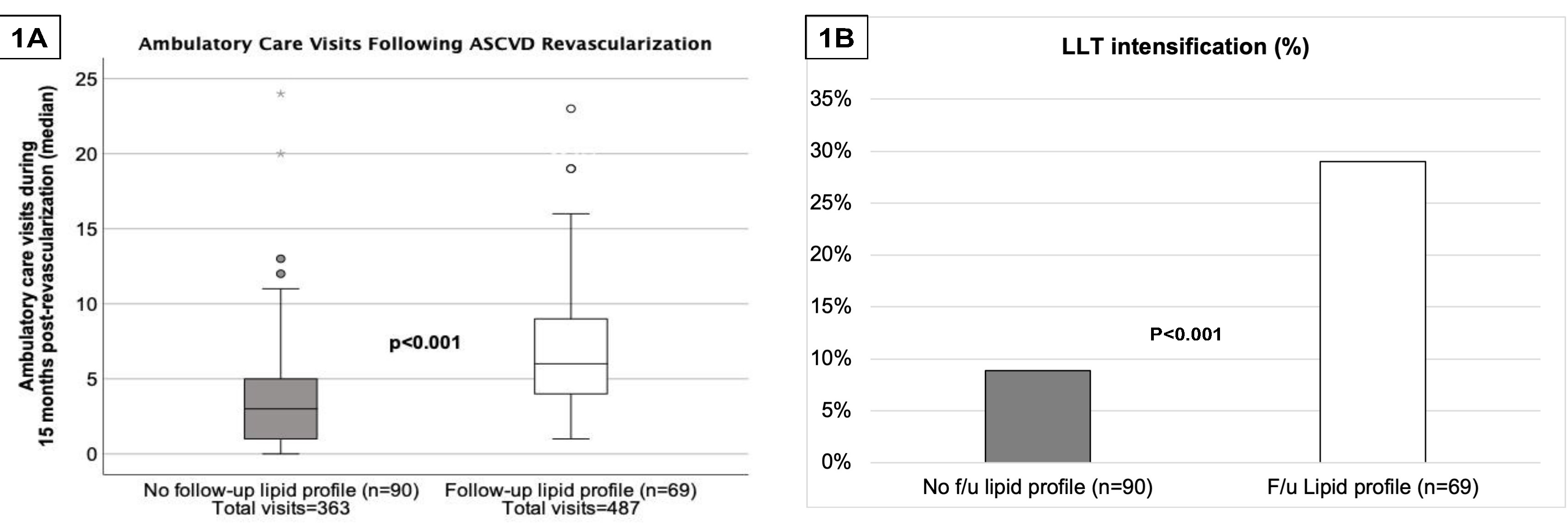
Goals: Evaluate the number of ambulatory care (AC) visits at which follow-up lipid profiles and/or LLT intensification failed to occur (e.g., missed opportunity) following revascularization in patients with ASCVD.
Methods: We report a retrospective cohort study evaluating lipid management following revascularization for ASCVD of the coronary, cerebral, or peripheral arteries between July 2021 – July 2022. Patients were identified from procedure lists. Exclusion criteria included baseline LDL-C < 70 mg/dl, triglycerides > 500 mg/dl, dialysis dependence, and no follow-up care within 6 months of revascularization. The number of AC visits with a provider and LLT intensification following revascularization were compared between patients with a follow-up lipid panel versus those without within 15 months post-revascularization. Logistic regression was performed to identify characteristics associated with obtaining a follow-up lipid profile.
Results: Of the 159 patients included, 69 (43%) had a follow-up lipid panel for evaluation at an average of 162±115 days after revascularization; 35 (22% of the entire cohort) achieved an LDL <70 mg/dL. Patients with a follow-up lipid panel had significantly more AC visits and had higher rates of LLT intensification than those without follow-up lipids (Figure). Among the 90 patients without follow-up lipid profiles, there were a total of 363 missed opportunities to reassess lipids. Follow-up with either cardiology (OR 5.8 [95% CI 1.4-24.2]) or primary care (OR 4.1 [95% CI 1.8-9.3]) and diabetes (OR 2.7 [95% CI 1.2-5.9]) were positively associated with follow-up lipids; follow-up with vascular surgery (OR 0.2 [95% CI 0.0-0.9]), and heart failure (OR 0.2 [95% CI 0.1-0.8]) or CKD (OR 0.4 [95% CI 0.2-1.0]) were negatively associated with follow-up lipid panels.
Conclusion: Post-revascularization care of high-risk ASCVD patients is suboptimal; we identified many missed opportunities to reassess lipids and intensify LLT.
More abstracts on this topic:
Shahzad Zoha, Batool Asma, Ijaz Osama, Rao Asad Gul, Rasool Warda, Wani Shariq Ahmad, Rauf Faateh, Ilmaguook Badr, Khan Arslan Ahmed, Bhatti Ali Hanif
A transformative LDL cholesterol–lowering in vivo CRISPR gene editing medicine that functionally upregulates LDLR in mice and non-human primatesNewmark Judith, Raghav Jimit, Jaskolka Michael, Diner Benjamin, Soman Vikram, Jinadasa Tushare, Apte Ameya, Wu Meng, Bottega Steve, Thakkar Mansi, Agosto Luis, Wrighton Paul, Majithia Deep, Jambard Shreya, Jansson-fritzberg Linnea, Jones Mark, Fletcher Jillian, Weiss Mckenzie, Kaye Emily, Steward Briana, Bochicchio James, Pietrasiewicz Stephen, Iovino Salvatore, Marco Rubio Eugenio, Trong Phan Huu, Chander Nisha, Kazemian Mohammadreza, Lam Kieu, Reid Steve, Dinsmore Michael, Teslovich Tanya, Xie Jenny, Gupta Anshul, Amin Parth, Burkly Linda, Thompson Morgan, Rizal Salu, Bilodeau Maxime, Dong Ruhong, Zhen Wei