Final ID: Su1148
Association Between Diabetes and 5-year Mortality and Major Amputation Outcomes After Revascularization in Chronic Limb-threatening Ischemia
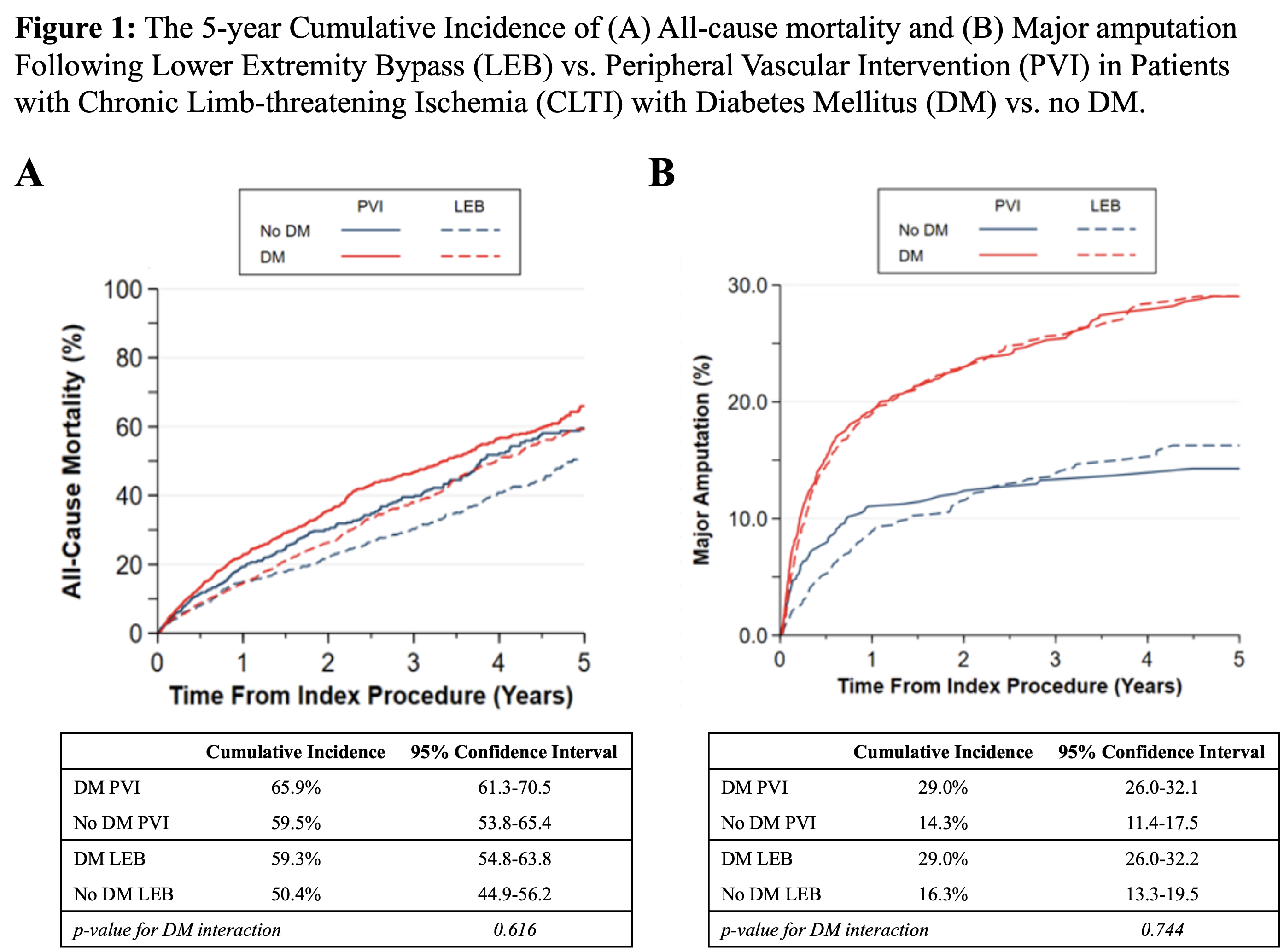
Abstract Body (Do not enter title and authors here): Introduction: Diabetes affects over 60% of patients with chronic limb-threatening ischemia (CLTI). The impact of diabetes mellitus (DM) in long-term outcomes after lower-extremity bypass (LEB) or peripheral vascular interventions (PVI) remains unclear. We aim to assess the association between DM and 5-year all-cause mortality and major amputation after LEB vs. PVI for CLTI.
Methods: Patients with CLTI undergoing LEB or PVI between 2014-2019 were abstracted from the Vascular Quality Initiative registry and stratified by DM status. Mortality and major amputation outcomes were derived from Medicare claims data. Patients in LEB vs. PVI groups were 1:1 propensity matched based on 13 preprocedural variables. The 5-year cumulative incidence of mortality by revascularization group and DM status was assessed with Kaplan-Meier and the risk in patients with DM vs. no DM by revascularization group (i.e., interaction DM status*revascularization group) was tested using Cox proportional hazard regression model. The Aalen-Johansen method and Fine-Gray model assessed the 5-year cumulative incidence and interaction between DM status and revascularization accounting for the competing risk of mortality.
Results: A total of 4,210 patients (mean age 70.9 ±10.9, 30.7% female) were included of whom patients with DM were 65.7% and 58.8% of the PVI and LEB groups, respectively. Mortality cumulative incidence at 5-years was higher for DM vs. no DM in PVI (65.9% vs 59.5%; p=0.022) and LEB (59.3% vs 50.4%; p=0.003), with non-significant interaction for DM status (p =0.616). Amputation risk at 5 years was higher for DM vs. no DM for PVI (29.0% vs 14.3%; p<0.001) and LEB (29.0% vs 16.3%; p<0.001), with non-significant interaction for DM status (p =0.744).
Conclusion: Mortality and major amputation risk at 5 years after revascularization for CLTI was higher for patients with DM vs. no DM regardless of the type of revascularization, with 3 out of 5 patients deceased and 1 out of 3 with a major amputation at 5 years. Shared decision-making and life expectancy discussions are needed for planning a definitive revascularization strategy.
Methods: Patients with CLTI undergoing LEB or PVI between 2014-2019 were abstracted from the Vascular Quality Initiative registry and stratified by DM status. Mortality and major amputation outcomes were derived from Medicare claims data. Patients in LEB vs. PVI groups were 1:1 propensity matched based on 13 preprocedural variables. The 5-year cumulative incidence of mortality by revascularization group and DM status was assessed with Kaplan-Meier and the risk in patients with DM vs. no DM by revascularization group (i.e., interaction DM status*revascularization group) was tested using Cox proportional hazard regression model. The Aalen-Johansen method and Fine-Gray model assessed the 5-year cumulative incidence and interaction between DM status and revascularization accounting for the competing risk of mortality.
Results: A total of 4,210 patients (mean age 70.9 ±10.9, 30.7% female) were included of whom patients with DM were 65.7% and 58.8% of the PVI and LEB groups, respectively. Mortality cumulative incidence at 5-years was higher for DM vs. no DM in PVI (65.9% vs 59.5%; p=0.022) and LEB (59.3% vs 50.4%; p=0.003), with non-significant interaction for DM status (p =0.616). Amputation risk at 5 years was higher for DM vs. no DM for PVI (29.0% vs 14.3%; p<0.001) and LEB (29.0% vs 16.3%; p<0.001), with non-significant interaction for DM status (p =0.744).
Conclusion: Mortality and major amputation risk at 5 years after revascularization for CLTI was higher for patients with DM vs. no DM regardless of the type of revascularization, with 3 out of 5 patients deceased and 1 out of 3 with a major amputation at 5 years. Shared decision-making and life expectancy discussions are needed for planning a definitive revascularization strategy.
More abstracts on this topic:
Adiponectin and Adiponectin/Leptin Ratio Associate with Cardiometabolic Risk in South Asian Americans: Updates from the MASALA Study
Uttarwar Salil, Shah Nilay, Kanaya Alka, Gadgil Meghana
Acculturation Class Influences Physical Activity Among African Immigrants Living with Diabetes and/or Hypertension: A Qualitative AnalysisOsokpo Onome, Bracy Danny, Adeniji Dolapo, Bankole Ayomide Okanlawon, Lewis Lisa, Riegel Barbara