Final ID: MDP666
Catheter-Directed Interventions for High-Risk Acute Pulmonary Embolism in patients with Liver Cirrhosis
Abstract Body (Do not enter title and authors here): Background: Catheter-Directed Interventions (CDIs) for Acute Pulmonary Embolism (PE) have been available for years. However, their use and effectiveness in patients with a concomitant diagnosis of liver cirrhosis is uncertain due to a paucity of data in this high-risk population. In this study, we aim to evaluate the safety, efficacy, and current trends in the use of CDIs for high-risk PE (HR-PE) in patients with liver cirrhosis.
Methods: Nationwide Readmissions Database (2016-2021) was used to identify patients with liver cirrhosis presenting with HR-PE (shock, pressor or mechanical circulatory support requirement). Patients who received systematic thrombolysis were excluded. Mahalanobis Distance Matching within the Propensity Score Caliper was used to match patients who received CDIs vs those who did not recieve any catheter-directed intervention. Inverse Probability weighting (IPW) was utilized, and Pearson’s chi-squared test was applied to the PSM-2 matched cohorts to compare outcomes.
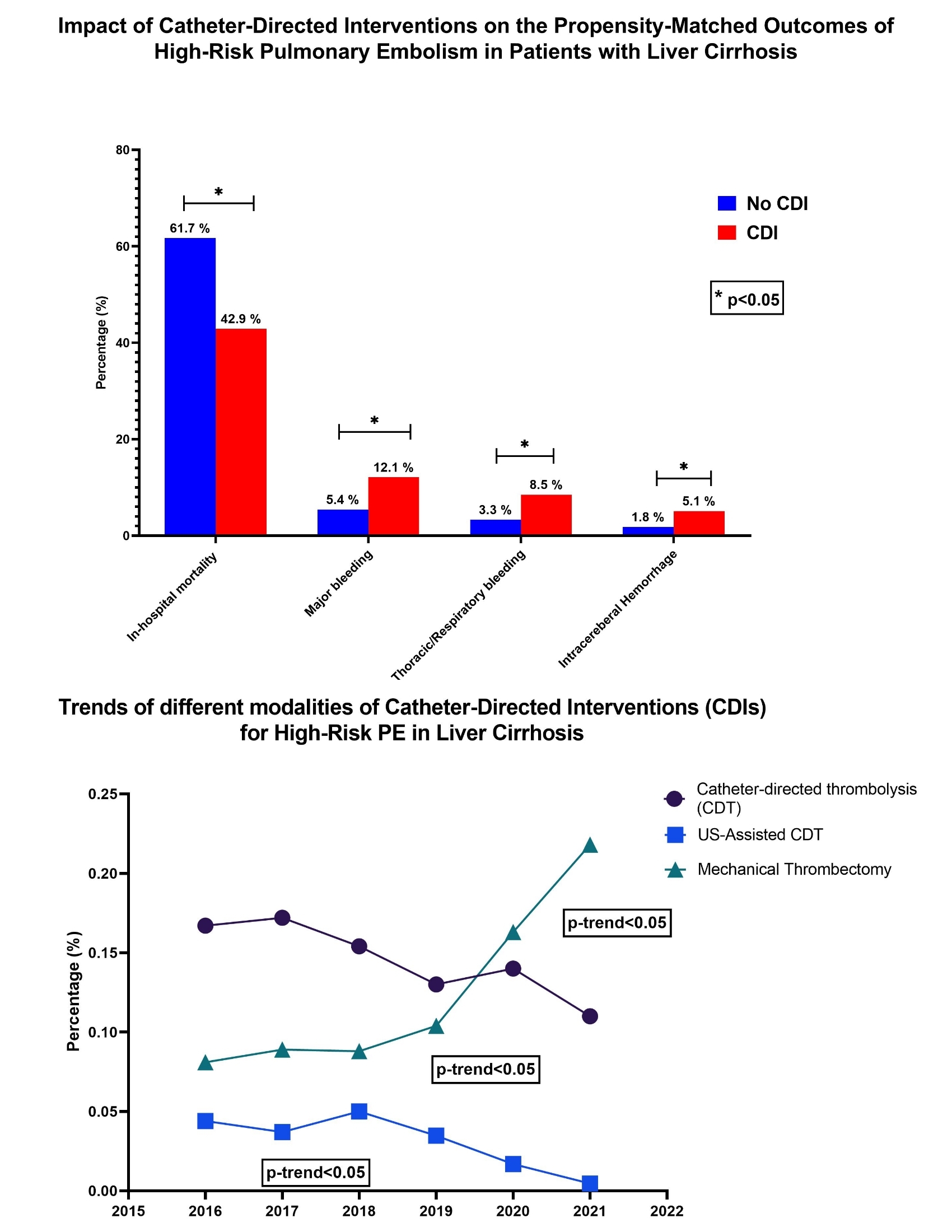
Results: Among 427,802 hospitalizations of patients with HR-PE and concomitant diagnosis of liver cirrhosis, only 1,319 (0.3%) of the patients underwent CDI. After propensity matching (N: 668 in each group), patients receiving CDI had a significantly lower mortality (42.9% vs. 61.7%, aOR:0.44, p <0.001). However, bleeding complications including major bleeding (12.1% vs 5.4%, aOR:1.9, p<0.001), thoraco-respiratory bleeding (8.5% vs 3.3%, aOR:1.9, p <0.001) and intracerebral hemorrhage (5.1% vs 1.8%, aOR:2.3, p:0.001) was higher in patients receiving CDIs. Short-term (30-day) readmission rates were lower in cirrhotic patients receiving CDI (12.4% vs 18.8%, p: 0.024). From 2016-2021, mortality associated with HR-PE in cirrhotic patients has not changed significantly (mean: 61.2%, p >0.05). There has been increasing use of mechanical thrombectomy (MT) over thrombolysis in recent years (0.08% to 0.22%, p-trend <0.001).
Conclusion: CDIs for HR-PE in patients with liver cirrhosis are rare and areassociated with significant reduction in mortality at the expense of higher bleeding risk. Despite a slight increase in the utilization of mechanical thrombectomy, mortality has not significantly decreased over the years.
Methods: Nationwide Readmissions Database (2016-2021) was used to identify patients with liver cirrhosis presenting with HR-PE (shock, pressor or mechanical circulatory support requirement). Patients who received systematic thrombolysis were excluded. Mahalanobis Distance Matching within the Propensity Score Caliper was used to match patients who received CDIs vs those who did not recieve any catheter-directed intervention. Inverse Probability weighting (IPW) was utilized, and Pearson’s chi-squared test was applied to the PSM-2 matched cohorts to compare outcomes.
Results: Among 427,802 hospitalizations of patients with HR-PE and concomitant diagnosis of liver cirrhosis, only 1,319 (0.3%) of the patients underwent CDI. After propensity matching (N: 668 in each group), patients receiving CDI had a significantly lower mortality (42.9% vs. 61.7%, aOR:0.44, p <0.001). However, bleeding complications including major bleeding (12.1% vs 5.4%, aOR:1.9, p<0.001), thoraco-respiratory bleeding (8.5% vs 3.3%, aOR:1.9, p <0.001) and intracerebral hemorrhage (5.1% vs 1.8%, aOR:2.3, p:0.001) was higher in patients receiving CDIs. Short-term (30-day) readmission rates were lower in cirrhotic patients receiving CDI (12.4% vs 18.8%, p: 0.024). From 2016-2021, mortality associated with HR-PE in cirrhotic patients has not changed significantly (mean: 61.2%, p >0.05). There has been increasing use of mechanical thrombectomy (MT) over thrombolysis in recent years (0.08% to 0.22%, p-trend <0.001).
Conclusion: CDIs for HR-PE in patients with liver cirrhosis are rare and areassociated with significant reduction in mortality at the expense of higher bleeding risk. Despite a slight increase in the utilization of mechanical thrombectomy, mortality has not significantly decreased over the years.
More abstracts on this topic:
Activation of prostaglandin E receptor 4 attenuates pulmonary vascular remodeling and pulmonary hypertension in monocrotaline-exposed rats via non-inflammatory pathway
Kimuro Keiji, Yoshida Keimei, Izumi Ryo, Imabayashi Misaki, Masaki Kohei, Hosokawa Kazuya, Abe Kohtaro
Catheter-Directed Intervention for High-Risk Acute Pulmonary Embolism in Chronic Kidney DiseaseKumar Manoj, Ricciardi Mark, Arman Qamar, Ali Shafaqat, Jamshed Aneeza, Murthi Mukunthan, Kumar Nomesh, Kumar Sanjay, Kumari Rinkle, Alraies M Chadi, Gomez Valencia Javier