Final ID: MDP1217
Impella in Myocardial Infarction Complicated by Cardiogenic Shock: A Meta-Analysis
Abstract Body (Do not enter title and authors here): Background:
Despite recent technological advancements, myocardial infarction complicated with cardiogenic shock is associated with high mortality. Impella has been advocated as an adjunct to the standard of care, but conflicting data has hindered greater utilization. We performed an updated meta-analysis with the recent data.
Methods:
We searched PubMed and Embase, screened 787 articles, and identified twelve studies that met eligibility criteria; these randomized controlled trials and cohort studies compared Impella to other mechanical circulatory support systems in patients with myocardial infarction complicated by cardiogenic shock. We evaluated groups with twenty-three metrics related to adverse events and clinical outcomes. A random effects model assessed heterogeneity between studies.
Results:
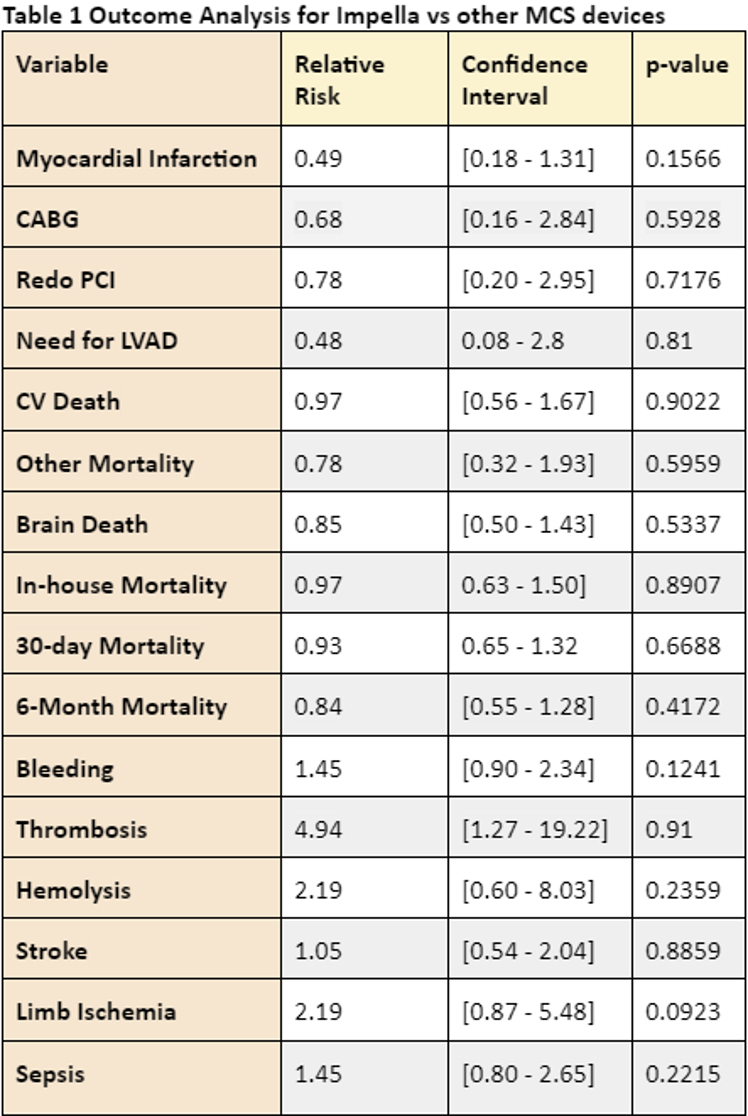
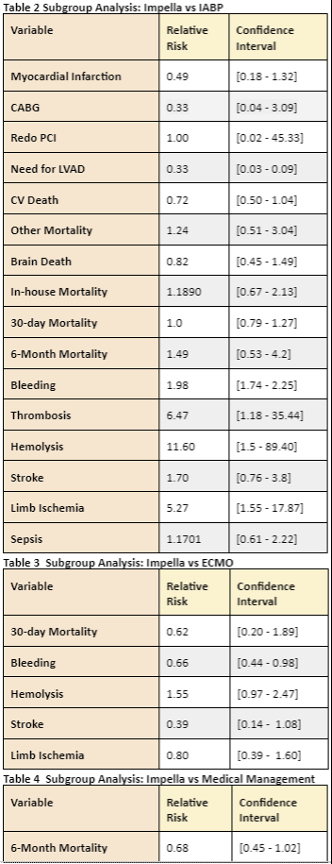
We did not find a statistically significant difference between groups across all twenty-three included metrics: in-house mortality, 30-day mortality, 6-month mortality, brain death, cardiovascular death, non-cardiac mortality, myocardial infarction, need for repeat percutaneous coronary intervention, need for left ventricular assist device, coronary bypass artery graft, stroke, limb ischemia, hemolysis, major bleeding, thrombosis, and sepsis. Table 1 Our subgroup analyses for intra-aortic balloon pump, extracorporeal membrane oxygenation, and medical management revealed similar results for mortality. In terms of bleeding, IABP was associated with better outcomes whereas ECMO was associated with worse outcomes than Impella. Impella was also associated with an increased risk of thrombosis as compared to IABP. Table 2,3,4
Conclusions:
Our updated meta-analysis did not relate Impella use to better outcomes. Heterogeneity in the timing of device implantation calls for stricter reporting in subsequent larger, randomized controlled trials.
Despite recent technological advancements, myocardial infarction complicated with cardiogenic shock is associated with high mortality. Impella has been advocated as an adjunct to the standard of care, but conflicting data has hindered greater utilization. We performed an updated meta-analysis with the recent data.
Methods:
We searched PubMed and Embase, screened 787 articles, and identified twelve studies that met eligibility criteria; these randomized controlled trials and cohort studies compared Impella to other mechanical circulatory support systems in patients with myocardial infarction complicated by cardiogenic shock. We evaluated groups with twenty-three metrics related to adverse events and clinical outcomes. A random effects model assessed heterogeneity between studies.
Results:
We did not find a statistically significant difference between groups across all twenty-three included metrics: in-house mortality, 30-day mortality, 6-month mortality, brain death, cardiovascular death, non-cardiac mortality, myocardial infarction, need for repeat percutaneous coronary intervention, need for left ventricular assist device, coronary bypass artery graft, stroke, limb ischemia, hemolysis, major bleeding, thrombosis, and sepsis. Table 1 Our subgroup analyses for intra-aortic balloon pump, extracorporeal membrane oxygenation, and medical management revealed similar results for mortality. In terms of bleeding, IABP was associated with better outcomes whereas ECMO was associated with worse outcomes than Impella. Impella was also associated with an increased risk of thrombosis as compared to IABP. Table 2,3,4
Conclusions:
Our updated meta-analysis did not relate Impella use to better outcomes. Heterogeneity in the timing of device implantation calls for stricter reporting in subsequent larger, randomized controlled trials.
More abstracts on this topic:
Association between Pressure-Adjusted Heart Rate and Mortality in Cardiogenic Shock
Ginder Curtis, Jentzer Jacob, Guo Jianping, Van Diepen Sean, Katz Jason, Morrow David, Berg David
A Novel Subcellular β-arrestin Biased Allosteric ModulatorAnderson Preston, Rajagopal Sudarshan