Final ID: Su3067
Unraveling the Enigma of Acute Myocardial Infarction-Related Mortality in Malignancy Among Older Adults (≥65 years), A Decadal Dive into U.S Trends (1999-2020): A CDC WONDER Database Analysis
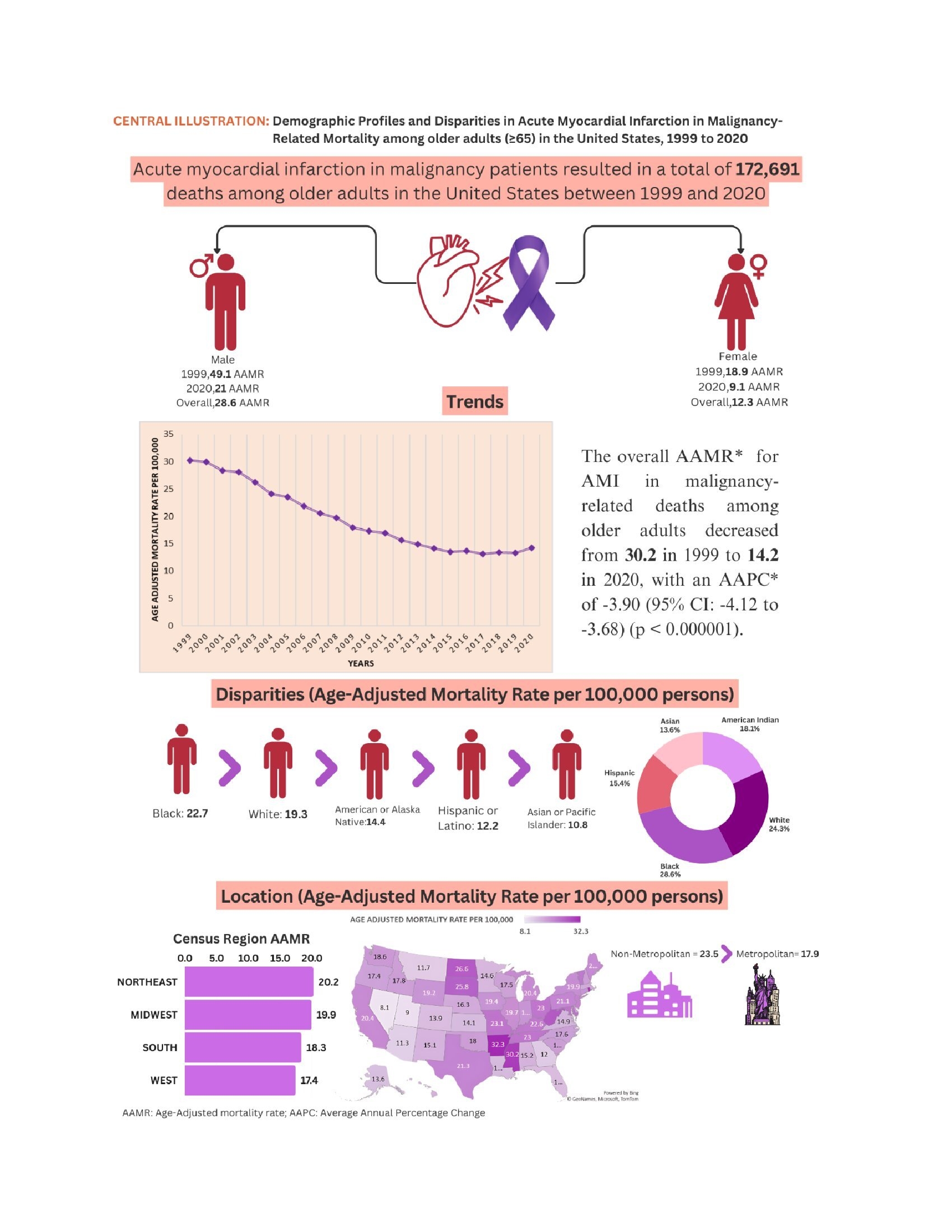
Abstract Body (Do not enter title and authors here): Background: Acute Myocardial Infarction (AMI) in malignancy is a significant cause of mortality globally. This study analyzed demographic trends and disparities in mortality rates due to AMI in malignancy among adults aged 65 and older from 1999 to 2020.
Methods: A retrospective analysis was performed using death certificate data from the Centers for Disease Control and Prevention database from 1999 to 2020. The analysis utilized ICD* codes I21 for AMI and C00-C97 for malignancies. Age-adjusted mortality rates (AAMRs) were calculated per 100,000 persons, and trends were assessed using Average Annual Percentage Change (AAPC) and annual percent change (APC). Data were stratified by year, sex, race/ethnicity, and geographical regions.
Results: Between 1999 and 2020, AMI in malignancy caused 172,691 deaths among U.S. older adults aged ≥65 years. The majority of deaths occurred in medical facilities (56.9%) and at decedents’ homes (24.2%). The overall AAMR for AMI in malignancy-related deaths decreased from 30.2 in 1999 to 14.2 in 2020, with an AAPC of -3.90 (p < 0.000001). Men showed higher AAMRs than women (28.6 vs. 12.3), with a more pronounced decrease in men (AAPC: -4.22, p < 0.000001) compared to women (AAPC: -3.78, p < 0.000001). Racial disparities were significant, with Black individuals having the highest AAMR (22.7), followed by Whites (19.3), American Indians or Alaska Natives (14.4), Hispanics (12.2), and Asians or Pacific Islanders (10.8). The decline in AAMR throughout the study was most pronounced in Black individuals (AAPC: -4.30, p < 0.000001). Geographically, the highest AAMRs were observed in Arkansas (32.3) and the lowest in Nevada (8.1). The Northeastern U.S. had the highest regional AAMR (20.2), followed by the Midwest (19.9), South (18.3), and West (17.4). Nonmetropolitan areas had higher AAMRs than metropolitan areas, though both saw significant declines from 1999 to 2020 (Metropolitan: AAPC: -3.97, p < 0.000001; Nonmetropolitan: AAPC: -2.64, p < 0.000001).
Conclusion: This study reveals significant demographic disparities in mortality rates related to AMI in malignant older adults. These findings emphasize the need for targeted interventions and improved access to care to reduce mortality and enhance outcomes in this vulnerable population.
Methods: A retrospective analysis was performed using death certificate data from the Centers for Disease Control and Prevention database from 1999 to 2020. The analysis utilized ICD* codes I21 for AMI and C00-C97 for malignancies. Age-adjusted mortality rates (AAMRs) were calculated per 100,000 persons, and trends were assessed using Average Annual Percentage Change (AAPC) and annual percent change (APC). Data were stratified by year, sex, race/ethnicity, and geographical regions.
Results: Between 1999 and 2020, AMI in malignancy caused 172,691 deaths among U.S. older adults aged ≥65 years. The majority of deaths occurred in medical facilities (56.9%) and at decedents’ homes (24.2%). The overall AAMR for AMI in malignancy-related deaths decreased from 30.2 in 1999 to 14.2 in 2020, with an AAPC of -3.90 (p < 0.000001). Men showed higher AAMRs than women (28.6 vs. 12.3), with a more pronounced decrease in men (AAPC: -4.22, p < 0.000001) compared to women (AAPC: -3.78, p < 0.000001). Racial disparities were significant, with Black individuals having the highest AAMR (22.7), followed by Whites (19.3), American Indians or Alaska Natives (14.4), Hispanics (12.2), and Asians or Pacific Islanders (10.8). The decline in AAMR throughout the study was most pronounced in Black individuals (AAPC: -4.30, p < 0.000001). Geographically, the highest AAMRs were observed in Arkansas (32.3) and the lowest in Nevada (8.1). The Northeastern U.S. had the highest regional AAMR (20.2), followed by the Midwest (19.9), South (18.3), and West (17.4). Nonmetropolitan areas had higher AAMRs than metropolitan areas, though both saw significant declines from 1999 to 2020 (Metropolitan: AAPC: -3.97, p < 0.000001; Nonmetropolitan: AAPC: -2.64, p < 0.000001).
Conclusion: This study reveals significant demographic disparities in mortality rates related to AMI in malignant older adults. These findings emphasize the need for targeted interventions and improved access to care to reduce mortality and enhance outcomes in this vulnerable population.
More abstracts on this topic:
Acoramidis Reduces All-Cause Mortality (ACM) and Cardiovascular-Related Hospitalization (CVH): Initial Outcomes From the ATTRibute-CM Open-Label Extension (OLE) Study
Judge Daniel, Masri Ahmad, Obici Laura, Poulsen Steen, Sarswat Nitasha, Shah Keyur, Soman Prem, Cao Xiaofan, Wang Kevin, Pecoraro Maria, Tamby Jean-francois, Gillmore Julian, Katz Leonid, Fox Jonathan, Maurer Mathew, Alexander Kevin, Ambardekar Amrut, Cappelli Francesco, Fontana Marianna, Garcia-pavia Pablo, Grogan Martha, Hanna Mazen
Assessing Coronary Artery Disease Severity: Leveraging Inflammatory Markers As a Prognostic IndicatorsTurnbull Scott, Dugal Jasmine, Gill Randeep, Wang Shawn, Cross Chad, Mubder Mohamad