Final ID: Su2174
Validation of an Unsupervised Cluster Model of Clinical and Echocardiographic characteristics for Natural Unbiased Stratification of Risk In Heart Failure with Preserved Ejection Fraction
Abstract Body (Do not enter title and authors here): Background: We previously reported computational clustering to describe clinically distinct phenotypes of heart failure with preserved ejection fraction (HFpEF). We aimed to validate our prior model exploring the clinical and echocardiographic variations in HFpEF on unseen dataset.
Methods: Retrospectively, 556 HFpEF patients previously reported [exploration group, Age: 66±17years , 56%females, EF: 63±6%, DOI:10.1016/s0735-1097(19)31580-3] and a new unseen dataset of 1055 HFpEF patients [validation group, Age: 58±17years , 56% females, EF: 60±6%] were studied and followed for a median of 4.7 years for death and cardiac hospitalization. A 2-step unsupervised cluster model previously applied to the exploratory group and composed of 11 echo and clinical variables (age, sex, diabetes, hypertension, hematocrit, creatinine, pulmonary functions, E/A ratio, E/e’ ratio, left atrial volume index, tricuspid regurgitation velocity) was saved and applied to the unseen validation dataset. Clusters were described based on echo and clinical domains.
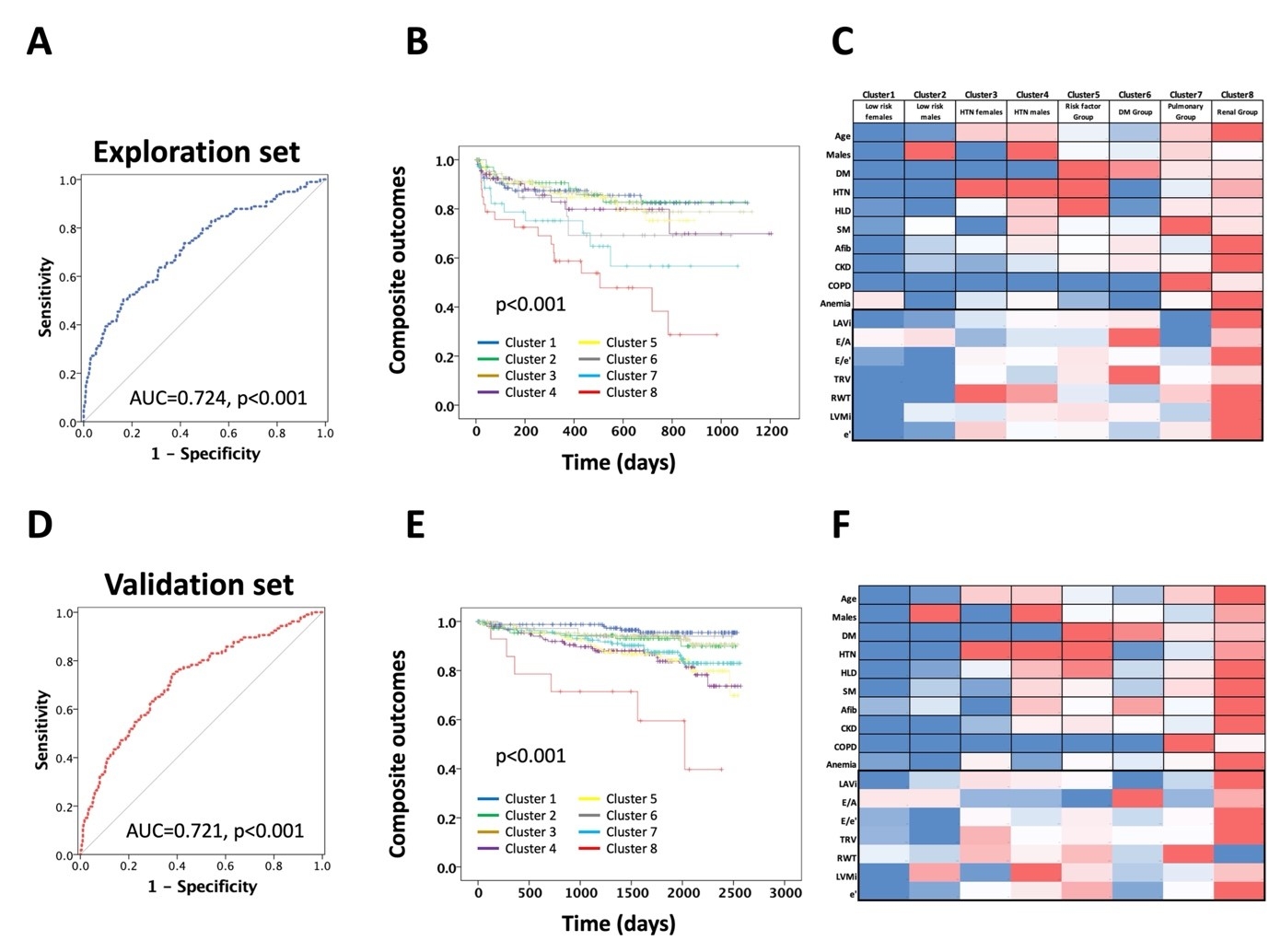
Results: The analysis in the exploratory group yielded 8 different clusters with increasing distinct clinical, structural, hemodynamic, as well as adverse event risks as previously reported [low risk females (lowest risk), low risk males, hypertensive females, hypertensive males, multiple risk factor group, diabetes group, pulmonary group, and renal group (highest risk), figure 1 A,B,C]. When applied to the exploratory group, similar clinical, echocardiographic and event rate risk criteria were noted (figure 1 D,E,F). The diagnostic performance of both exploratory and validation models were comparable (AUC=0.724, 0.721, respectively). In the validation group, the clusters also differentiated brain natriuretic peptide and troponin concentration and had progressively worsening H2FPEF score, exercise capacity and exercise induced diastolic dysfunction.
Conclusion: The current study validates our previous model and confirms the previously reported heterogeneous clinical and echocardiographic phenotypes. Next, computational models such as the one reported should be applied to clinical trials to discover new therapeutic approaches unique to each phenotype.
Methods: Retrospectively, 556 HFpEF patients previously reported [exploration group, Age: 66±17years , 56%females, EF: 63±6%, DOI:10.1016/s0735-1097(19)31580-3] and a new unseen dataset of 1055 HFpEF patients [validation group, Age: 58±17years , 56% females, EF: 60±6%] were studied and followed for a median of 4.7 years for death and cardiac hospitalization. A 2-step unsupervised cluster model previously applied to the exploratory group and composed of 11 echo and clinical variables (age, sex, diabetes, hypertension, hematocrit, creatinine, pulmonary functions, E/A ratio, E/e’ ratio, left atrial volume index, tricuspid regurgitation velocity) was saved and applied to the unseen validation dataset. Clusters were described based on echo and clinical domains.
Results: The analysis in the exploratory group yielded 8 different clusters with increasing distinct clinical, structural, hemodynamic, as well as adverse event risks as previously reported [low risk females (lowest risk), low risk males, hypertensive females, hypertensive males, multiple risk factor group, diabetes group, pulmonary group, and renal group (highest risk), figure 1 A,B,C]. When applied to the exploratory group, similar clinical, echocardiographic and event rate risk criteria were noted (figure 1 D,E,F). The diagnostic performance of both exploratory and validation models were comparable (AUC=0.724, 0.721, respectively). In the validation group, the clusters also differentiated brain natriuretic peptide and troponin concentration and had progressively worsening H2FPEF score, exercise capacity and exercise induced diastolic dysfunction.
Conclusion: The current study validates our previous model and confirms the previously reported heterogeneous clinical and echocardiographic phenotypes. Next, computational models such as the one reported should be applied to clinical trials to discover new therapeutic approaches unique to each phenotype.
More abstracts on this topic:
A Case of Concomitant Wild-Type Transthyretin and Systemic Light Chain Amyloidosis Involving Separate Organs
Chiu Leonard, Afrough Aimaz, Nadeem Urooba, Jebakumar Deborah, Grodin Justin
Aberrant Regulation of endMT in Turner Syndrome: Implications for the Pathogenesis of Congenital Cardiovascular DiseaseGarcia Huitron Eric Ivan, Zhang Xiaoying, Babcock Lance, Grande-allen Kathryn, Prakash Siddharth