Final ID: MDP562
Mortality and Ventricular Support Use in Cardiogenic Shock between 2018-2023: A Report from the Northern New England Cardiovascular Disease Study Group
Abstract Body (Do not enter title and authors here): Background: Mortality from cardiogenic shock remains high, despite increasing awareness and multiple national initiatives to improve survival. Little is known about the relationship between support device use and overall survival in patients with cardiogenic shock. We sought to examine the temporal trends in mortality and ventricular support in patients with cardiogenic shock undergoing PCI in Northern New England.
Methods: The NNE registry was queried to identify patients presenting for PCI who manifest cardiogenic shock between 2018 and 2023. Shock was defined by the NCDR definition including sustained hypotension requiring ionopressor use. Demographics, procedural data, mortality and intraprocedural ventricular support device use was collected. Standard statistical methods were used to calculate outcomes and statistical significance.
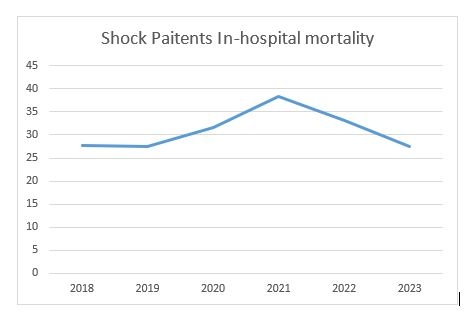
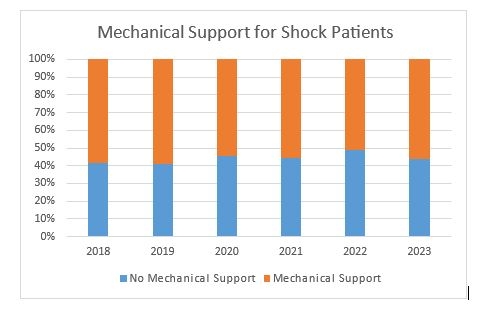
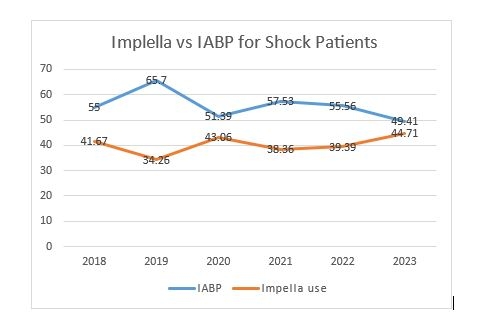
Results: At total of 842 patients were identified who presented with shock. Overall in-hospital mortality was 30.9%, and varied from 27.4% in 2018 to 38.3% in 2021 during the height of the COVID-19 pandemic (Image 1). Mechanical support use remained flat, with an average use of 57% of all cases (Image 2). The distribution of intra-aortic balloon pumps and Impella devices changed, with Impella use increasing from around 41% in 2018 to 44%and IABP use decreasing from 55% to around 49% by the end of the study in 2023 (Image 3). There was no correlation between survival and type of mechanical support device used.
Conclusions: Despite using ventricular support in nearly 60% of cases, in-hospital mortality for cardiogenic shock remains high at around 30%. A trend towards less IABP use and higher Impella use has not changed overall mortality. More study is needed to better understand how to optimize care for patients presenting with cardiogenic shock.
Methods: The NNE registry was queried to identify patients presenting for PCI who manifest cardiogenic shock between 2018 and 2023. Shock was defined by the NCDR definition including sustained hypotension requiring ionopressor use. Demographics, procedural data, mortality and intraprocedural ventricular support device use was collected. Standard statistical methods were used to calculate outcomes and statistical significance.
Results: At total of 842 patients were identified who presented with shock. Overall in-hospital mortality was 30.9%, and varied from 27.4% in 2018 to 38.3% in 2021 during the height of the COVID-19 pandemic (Image 1). Mechanical support use remained flat, with an average use of 57% of all cases (Image 2). The distribution of intra-aortic balloon pumps and Impella devices changed, with Impella use increasing from around 41% in 2018 to 44%and IABP use decreasing from 55% to around 49% by the end of the study in 2023 (Image 3). There was no correlation between survival and type of mechanical support device used.
Conclusions: Despite using ventricular support in nearly 60% of cases, in-hospital mortality for cardiogenic shock remains high at around 30%. A trend towards less IABP use and higher Impella use has not changed overall mortality. More study is needed to better understand how to optimize care for patients presenting with cardiogenic shock.
More abstracts on this topic:
Circulatory Support Devices in ST-Elevation MI Cardiogenic Shock Patients: Real-World Outcomes from Nationwide Inpatient Sample
Trivedi Jaimin, Gallo Michele, Samson Rohan, Fu Sheng, Arora Sonali, Moore Stephanie, Pahwa Siddharth, Slaughter Mark
Admission Acid-Base Status and Mortality in Cardiac Intensive Care Unit PatientsCanova Tyler, Lipps Kirsten, Hillerson Dustin, Kashani Kianoush, Dahiya Garima, Jentzer Jacob