Final ID: Su3096
Factors Associated with the Development of Incident Chronic Hypertension in the Postpartum Period: An Electronic Medical Record Analysis
Abstract Body (Do not enter title and authors here): Background: Hypertensive disorders of pregnancy (HDP), including preeclampsia and gestational hypertension, are associated with increased risk of cardiovascular disease (CVD) later in life. This effect is strongly mediated by the subsequent development of chronic hypertension (HTN). Our objective is to identify clinical factors associated with incident HTN in a racially diverse cohort of postpartum patients using electronic health record (EHR) data.
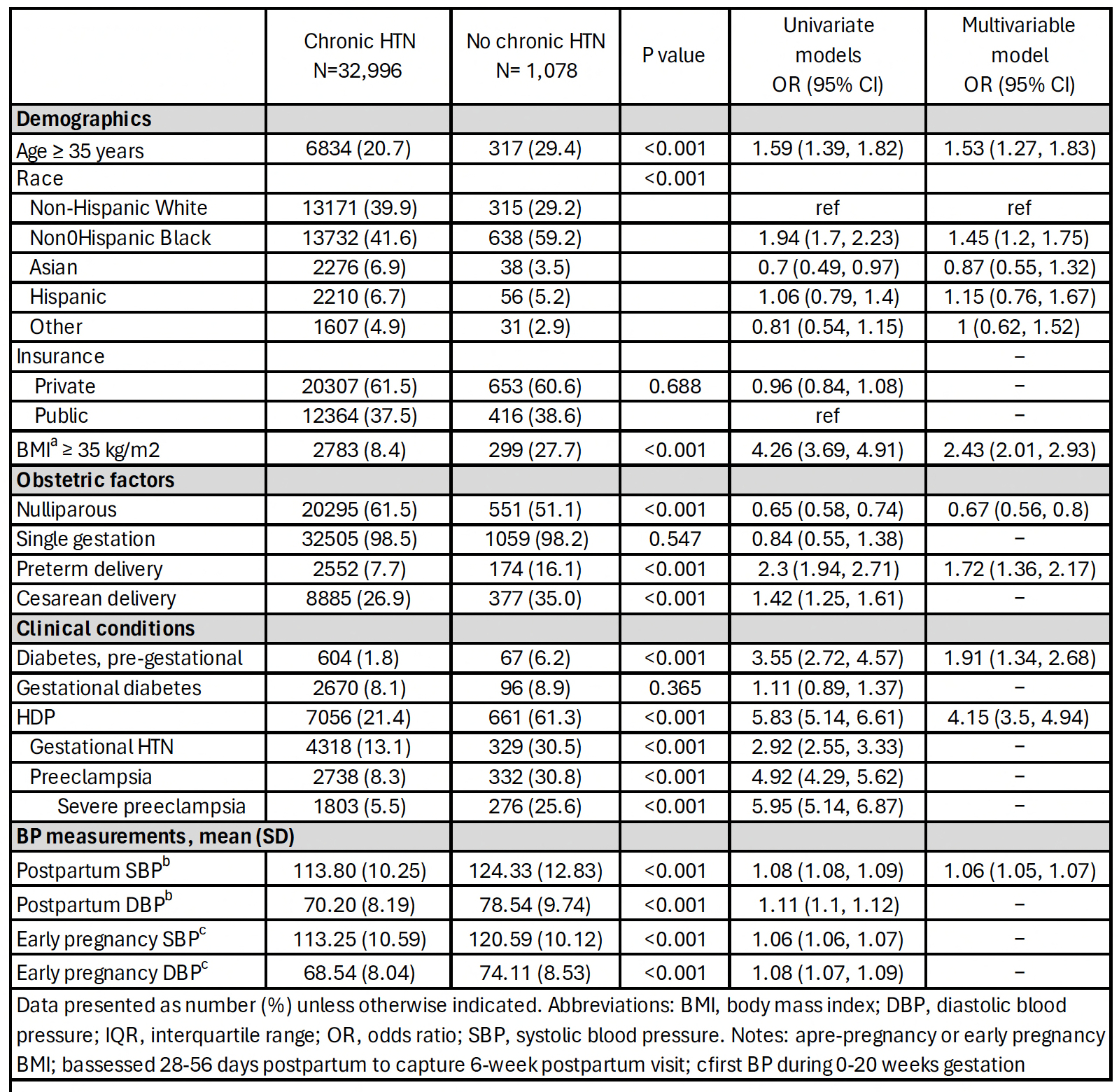
Methods: We identified patients with a delivery at Penn Medicine between 2012 and 2020 who did not have chronic HTN prior to delivery. The primary outcome was HTN between 6 and 24 months postpartum. HTN was identified based on ≥1 ICD code or ≥2 blood pressures (BP) ≥140/90. Univariable and multivariable logistic regression was used to model the association between patient factors assessed during pregnancy through the 6-week postpartum visit and incident HTN.
Results: In the final cohort of 34,074 unique patients, mean age was 29.6 years, 42% identified as Black, and 38% had Medicaid insurance. A total of 1,078 patients (3.2%) developed incident HTN between 6 and 24 months postpartum. HTN was more common in patients with HDP compared to those without HDP (8.6% vs. 1.6%, p< 0.001). Factors independently associated with HTN are listed in the Table. After adjusting for patient demographics and clinical factors, older maternal age, Black race (vs. White race), preterm birth, obesity, diabetes, HDP, and 6-week postpartum systolic BP (SBP) were associated with HTN. HDP (OR 3.8, 95% CI 3.2, 4.5) and pre-pregnancy BMI ≥35 kg/m2 (OR 2.2, 95% CI 1.8, 2.7) were associated with the highest odds of incident HTN. Every 1 mmHg increase in postpartum SBP was associated with a 6% higher odds of incident HTN, after adjusting for HDP and other clinical factors.
Conclusions: Patient factors that are routinely collected in the EHR, including HDP and BMI, are strongly associated with increased risk of developing incident HTN between 6-24 months postpartum in a racially diverse cohort. SBP at 6-weeks postpartum is an independent and underappreciated risk factor for HTN. Future work will develop and validate prediction models of incident postpartum HTN in this population at risk for CVD.
Methods: We identified patients with a delivery at Penn Medicine between 2012 and 2020 who did not have chronic HTN prior to delivery. The primary outcome was HTN between 6 and 24 months postpartum. HTN was identified based on ≥1 ICD code or ≥2 blood pressures (BP) ≥140/90. Univariable and multivariable logistic regression was used to model the association between patient factors assessed during pregnancy through the 6-week postpartum visit and incident HTN.
Results: In the final cohort of 34,074 unique patients, mean age was 29.6 years, 42% identified as Black, and 38% had Medicaid insurance. A total of 1,078 patients (3.2%) developed incident HTN between 6 and 24 months postpartum. HTN was more common in patients with HDP compared to those without HDP (8.6% vs. 1.6%, p< 0.001). Factors independently associated with HTN are listed in the Table. After adjusting for patient demographics and clinical factors, older maternal age, Black race (vs. White race), preterm birth, obesity, diabetes, HDP, and 6-week postpartum systolic BP (SBP) were associated with HTN. HDP (OR 3.8, 95% CI 3.2, 4.5) and pre-pregnancy BMI ≥35 kg/m2 (OR 2.2, 95% CI 1.8, 2.7) were associated with the highest odds of incident HTN. Every 1 mmHg increase in postpartum SBP was associated with a 6% higher odds of incident HTN, after adjusting for HDP and other clinical factors.
Conclusions: Patient factors that are routinely collected in the EHR, including HDP and BMI, are strongly associated with increased risk of developing incident HTN between 6-24 months postpartum in a racially diverse cohort. SBP at 6-weeks postpartum is an independent and underappreciated risk factor for HTN. Future work will develop and validate prediction models of incident postpartum HTN in this population at risk for CVD.
More abstracts on this topic:
Acute Bilateral Breast Swelling as a Rare Manifestation of Heart Failure Exacerbation: A Case Report
Mohyeldin Moiud, Anto Anandu, Hossain Muhammad
A Shocking Postpartum CourseWozniak Phillip, Grodzinsky Anna