Final ID: Su3095
Maternal Plasma Proteome: Associations with Blood Pressure during Pregnancy and Postpartum
Abstract Body (Do not enter title and authors here): INTRODUCTION
Pregnancy is marked by cardiovascular and hemodynamic changes to enable normal placental-fetal growth but may also predispose women to adverse outcomes including hypertensive disorders. Studies have assessed the plasma proteome of hypertension, but proteomic biomarkers of maternal blood pressure (BP) through pregnancy and postpartum remain unexplored.
OBJECTIVES
Explore the 1st trimester (TM) maternal plasma proteome in relation to systolic (S) and diastolic (D) BP in the 1st and 3rd third TM, and 3 months postpartum.
METHODS
We obtained baseline, 1st TM plasma samples from n=435 women from an antenatal multiple micronutrient vs iron-folic acid supplement trial in rural NW Bangladesh (West et al JAMA 2014). Phlebotomy occurred <12 wk gestation. Blood pressure was measured (mmHg) by trained staff with manual sphygmomanometers. Plasma specimens were shipped to Baltimore under liquid nitrogen, stored for ~10 years at -80oC before processing by SomaScan®, a synthetic aptamter-based assay that quantified relative abundance of 6,431 unique plasma proteins. We performed simple linear regression to correlate (r) protein abundance with SBP and DBP at each timepoint, adjusting for maternal age, body mass index, parity, and trial supplement allocation, defining significance as a false discovery rate (chance-corrected p-value, q) of q<0.05.
RESULTS
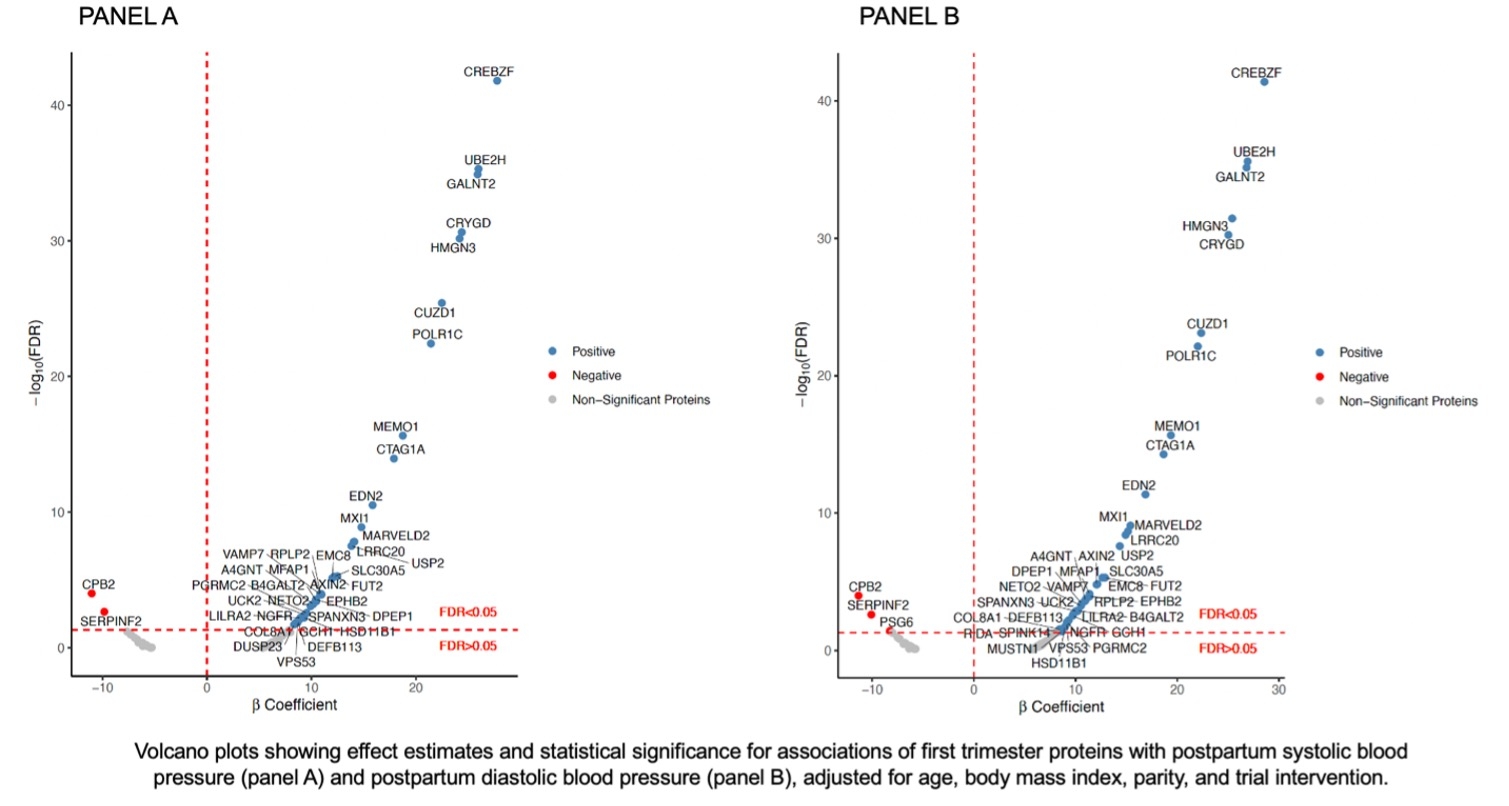
Six proteins (led by IGFBP-2, r=-0.22 and leptin, r=0.21), 2 proteins (NRP1, r=-0.22 and APOE, r=0.21) were correlated with 1st trimester, and 4 (LPLC1, APOF, OMGP, SLAF9) and zero proteins with 3rd trimester SBP and DBP, respectively (q<0.05). In contrast, 41 proteins were associated with both SBP and DBP at 3-month postpartum, 39 of which overlapped, of which 37 were positively correlated (ranges: r=0.62-0.17) (Figure1A and B). Proteins postpartum were different from 1st trimester. These included proteins involved in transcription (ex: CREBZF, GALNT2), cell proliferation (HMGN3, CUZD1), vascular function (UBE2H, EDN2), and inflammation (LIRA2).
CONCLUSIONS
Findings suggest that the maternal plasma proteome from the 1st TM is most aligned with cardiovascular tensive physiology of a non-pregnant (i.e., postpartum) person. BP during pregnancy itself (i.e. first and third TMs) may not follow the same pathways regulating it in the non-pregnant state (postpartum). The complex physiology of blood pressure regulation in pregnancy should be considered in studies exploring proteomics in pregnancy.
Pregnancy is marked by cardiovascular and hemodynamic changes to enable normal placental-fetal growth but may also predispose women to adverse outcomes including hypertensive disorders. Studies have assessed the plasma proteome of hypertension, but proteomic biomarkers of maternal blood pressure (BP) through pregnancy and postpartum remain unexplored.
OBJECTIVES
Explore the 1st trimester (TM) maternal plasma proteome in relation to systolic (S) and diastolic (D) BP in the 1st and 3rd third TM, and 3 months postpartum.
METHODS
We obtained baseline, 1st TM plasma samples from n=435 women from an antenatal multiple micronutrient vs iron-folic acid supplement trial in rural NW Bangladesh (West et al JAMA 2014). Phlebotomy occurred <12 wk gestation. Blood pressure was measured (mmHg) by trained staff with manual sphygmomanometers. Plasma specimens were shipped to Baltimore under liquid nitrogen, stored for ~10 years at -80oC before processing by SomaScan®, a synthetic aptamter-based assay that quantified relative abundance of 6,431 unique plasma proteins. We performed simple linear regression to correlate (r) protein abundance with SBP and DBP at each timepoint, adjusting for maternal age, body mass index, parity, and trial supplement allocation, defining significance as a false discovery rate (chance-corrected p-value, q) of q<0.05.
RESULTS
Six proteins (led by IGFBP-2, r=-0.22 and leptin, r=0.21), 2 proteins (NRP1, r=-0.22 and APOE, r=0.21) were correlated with 1st trimester, and 4 (LPLC1, APOF, OMGP, SLAF9) and zero proteins with 3rd trimester SBP and DBP, respectively (q<0.05). In contrast, 41 proteins were associated with both SBP and DBP at 3-month postpartum, 39 of which overlapped, of which 37 were positively correlated (ranges: r=0.62-0.17) (Figure1A and B). Proteins postpartum were different from 1st trimester. These included proteins involved in transcription (ex: CREBZF, GALNT2), cell proliferation (HMGN3, CUZD1), vascular function (UBE2H, EDN2), and inflammation (LIRA2).
CONCLUSIONS
Findings suggest that the maternal plasma proteome from the 1st TM is most aligned with cardiovascular tensive physiology of a non-pregnant (i.e., postpartum) person. BP during pregnancy itself (i.e. first and third TMs) may not follow the same pathways regulating it in the non-pregnant state (postpartum). The complex physiology of blood pressure regulation in pregnancy should be considered in studies exploring proteomics in pregnancy.
More abstracts on this topic:
A Study Using Team Based Hypertension Care Focused on Black Patients to Inform a Future Randomized Trial
Manandhar Srista, Taylor Yhenneko, Bosworth Hayden, Pokharel Yashashwi, Chhetri Sunit, Sutton Danielle, Saha Animita, Kaur Suneet, Brown Josh, Moore Justin, Callahan Kate, Williamson Jeff
A major effect of aprocitentan on albuminuria in patients with resistant hypertensionWeber Michael, Bakris George, Flack John, Gimona Alberto, Narkiewicz Krzysztof, Sassi-sayadi Mouna, Wang Jiguang, Schlaich Markus