Final ID: Su4019
Sodium Glucose Cotransporter 2 Inhibitors After Acute Myocardial Infarction: An updated systematic review and meta-analysis.
Abstract Body (Do not enter title and authors here): Background: Sodium-glucose co-transporter two inhibitors (SGLT2i) have recently been included in heart failure (HF) guidelines due to their benefits in reducing mortality and hospitalization rates. However, the benefits of SGLT2i in patients with post-acute myocardial infarction (MI) remain controversial. Therefore, we aim to perform an updated systematic review and meta-analysis comparing SGLT2i with placebo in patients after an acute MI.
Methods: We performed a systematic review and meta-analysis to determine the impact of SLGT2i in patients with post-acute MI with or without diabetes type II (DM II). We systematically searched Pubmed, Cochrane, and Embase for randomized controlled trials (RCTs) comparing SGLT2i and placebo in patients following an acute MI. The primary outcome assessed was (1) HF hospitalization. In this analysis, we also included the following secondary outcomes:(2) cardiovascular (CV) mortality and (3) MI recurrence. Risk Ratios(RRs) with 95% confidence interval (CI) were pooled across studies using a random effect model.
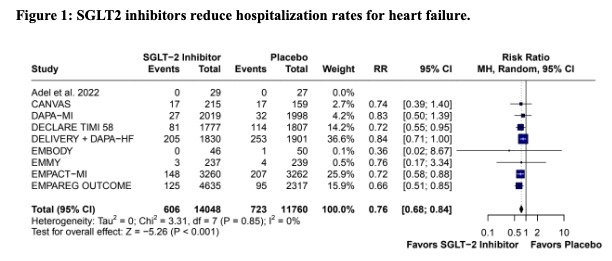
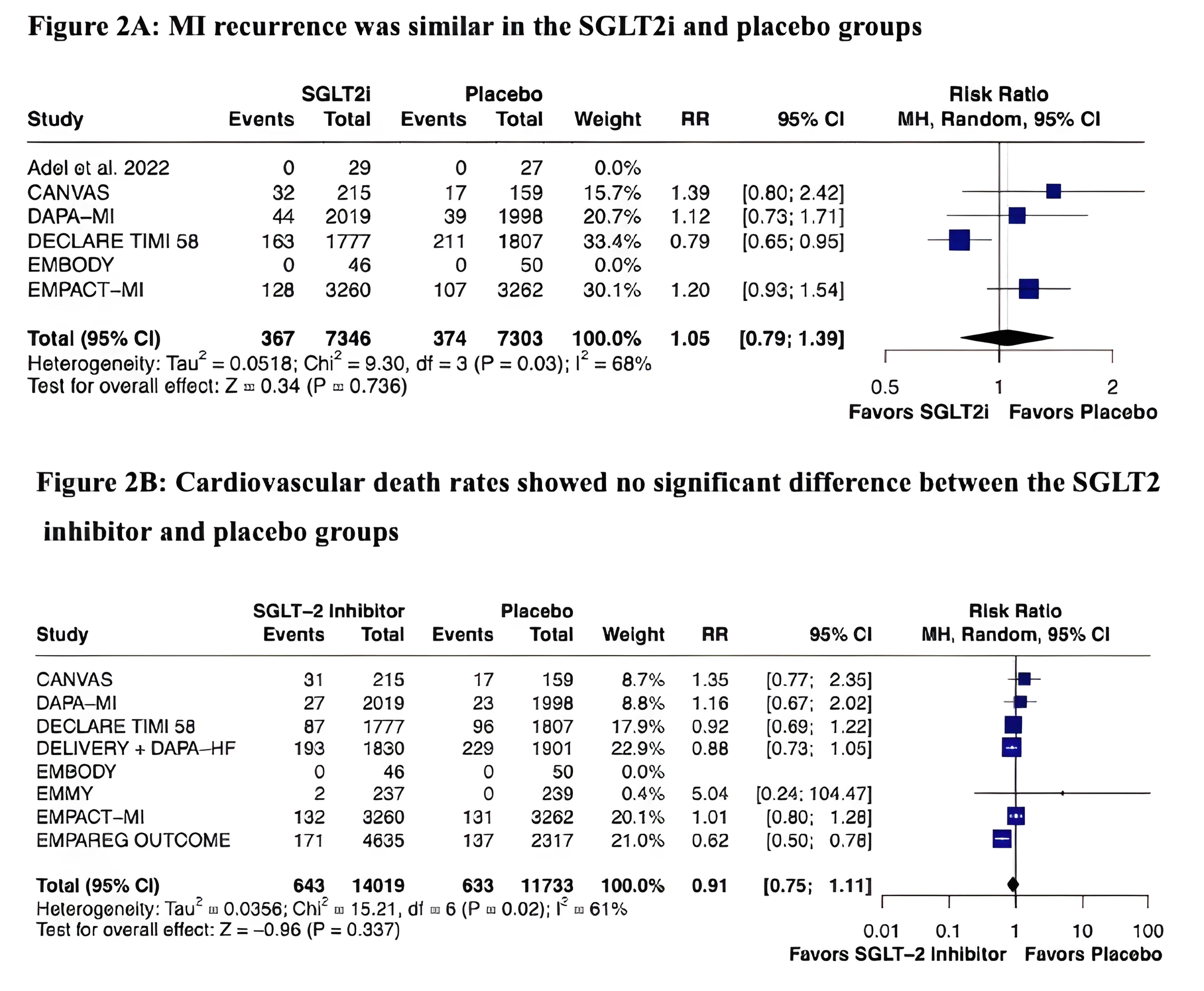
Results: Our meta-analysis included ten RCTs comprising 25908 patients, of whom 14098 (54.4%) received SGLT2i therapy and 15078 (58.2%) had type II diabetes. The mean age was 62 years, and the mean follow-up was 21.2 months. In the pooled analysis, HF hospitalization was significantly lower in the SGLT2is group (RR 0.76; 95%CI 0.68,0.84; p<0.001; Fig. 1). There was no statistically significant difference between the groups in terms of MI recurrence rates (RR 1.05; 95%CI 0.79,1.39; p=0.7; Fig. 2 A) and CV mortality (RR 0.91; 95%CI 0.75,1.11; p=0.34; Fig. 2 B).
Conclusion: In this updated meta-analysis of patients with a history of acute myocardial infarction, the administration of SGLT2i was significantly associated with reduced hospitalization rates for heart failure. However, our results show no benefits in MI recurrence and CV mortality endpoints.
Methods: We performed a systematic review and meta-analysis to determine the impact of SLGT2i in patients with post-acute MI with or without diabetes type II (DM II). We systematically searched Pubmed, Cochrane, and Embase for randomized controlled trials (RCTs) comparing SGLT2i and placebo in patients following an acute MI. The primary outcome assessed was (1) HF hospitalization. In this analysis, we also included the following secondary outcomes:(2) cardiovascular (CV) mortality and (3) MI recurrence. Risk Ratios(RRs) with 95% confidence interval (CI) were pooled across studies using a random effect model.
Results: Our meta-analysis included ten RCTs comprising 25908 patients, of whom 14098 (54.4%) received SGLT2i therapy and 15078 (58.2%) had type II diabetes. The mean age was 62 years, and the mean follow-up was 21.2 months. In the pooled analysis, HF hospitalization was significantly lower in the SGLT2is group (RR 0.76; 95%CI 0.68,0.84; p<0.001; Fig. 1). There was no statistically significant difference between the groups in terms of MI recurrence rates (RR 1.05; 95%CI 0.79,1.39; p=0.7; Fig. 2 A) and CV mortality (RR 0.91; 95%CI 0.75,1.11; p=0.34; Fig. 2 B).
Conclusion: In this updated meta-analysis of patients with a history of acute myocardial infarction, the administration of SGLT2i was significantly associated with reduced hospitalization rates for heart failure. However, our results show no benefits in MI recurrence and CV mortality endpoints.
More abstracts on this topic:
Absence of standard modifiable risk factors (SMuRF-less) among 5002 Middle Eastern patients with atherosclerotic cardiovascular disease: (Interim analysis from the Jo-SMuRF Study)
Aldalal'ah Mo'men, Hammoudeh Ayman, Hamza Ibrahem, Alqudah Mohammad, Khasawneh Hasan, Alomari Sawsan, Alomari Ahmad, H. Assaf Sarah, Zaqqa Ayah, Khatatbeh Moawiah
A Bridge from Sweet to Sour: A Case of Recurrent Myocardial Stunning in Diabetic KetoacidosisSatish Vikyath, Pargaonkar Sumant, Slipczuk Leandro, Schenone Aldo, Maliha Maisha, Chi Kuan Yu, Sunil Kumar Sriram, Borkowski Pawel, Vyas Rhea, Rodriguez Szaszdi David Jose Javier, Kharawala Amrin, Seo Jiyoung