Final ID: MDP1751
A Pilot Study of Post-Discharge Atrial Fibrillation Using a Novel Mobile Electrocardiography Monitoring Device
Research Question Do patients who experience in-hospital post-operative AF have recurrent arrhythmias in the 30 days post discharge?
Goals To characterize the burden of AF after hospital discharge using a wearable telemetry device.
Methods Patients enrolled in the CTSN PACeS trial were eligible for this sub-study. PACeS is a randomized trial of anticoagulation versus no-anticoagulation in patients with new-onset post-operative AF. Eligibility criteria include patients with new onset AF defined as AF > lasting 60 minutes or recurrent AF episodes within 7 days after CABG and before hospital discharge. All patients in this sub-study wore a 3-lead mobile telemetry device upon hospital discharge that provided continuous beat-to-beat data for 30 days. For this analysis, an AF event was counted if it was at least 30 seconds in duration.
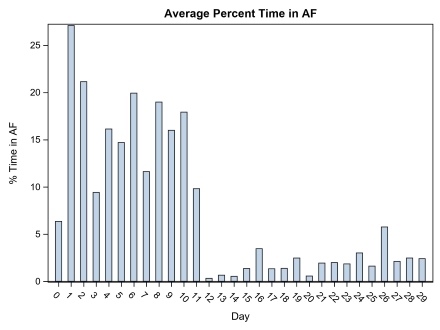
Results Forty-six patients participated in this sub-study. The mean age was 68.8 years, 21.7% were women, 78.3% White and 11% Hispanic. The mean and median device wear times were 23 and 29 days, respectively. The average total available analytic time (i.e., total time of interpretable electrocardiographic signal) was 20.3±3.3 hours/day. At least one episode of AF post-discharge was detected in 38 (82.6%) of patients. Among these, the median number of days in which patients had an episode of AF was 6. The mean duration of time in AF was 1.6±1.7 hours/day and the overall percent time in AF was 7.5%. Most patients (78.3%, n=36) had AF for <10% of the recording time. Nearly all AF events occurred within the first two weeks post discharge (Figure).
Conclusions In this telemetry study, patients who developed postoperative AF within 7 days of CABG were found to have a modest burden of post discharge AF episodes, most frequently within the first 2 weeks. These preliminary data should be verified in larger prospective studies, and may help inform anti-thrombotic and other management decisions for patients who develop AF following CABG surgery.
- Iribarne, Alexander ( Staten Island University Hospital /Northwell Health , Staten Island , New York , United States )
- Kramer, Robert ( Maine Medical Center , Portland , Maine , United States )
- Moquete, Ellen ( Icahn School of Medicine at Mount Sinai , New York , New York , United States )
- Hupf, Jonathan ( Icahn School of Medicine at Mount Sinai , New York , New York , United States )
- Duncan, Prezley ( Dartmouth Health , Lebanon , New Hampshire , United States )
- Mihelis, Efstathia ( Lenox Hill Hospital/Northwell Health , New York , New York , United States )
- Borger, Michael ( Leipzig Heart Center , Leipzig , Germany )
- Muir, Andrew ( Liverpool Heart and Chest Hospital , Liverpool , United Kingdom )
- Starnes, Vaughn ( University of Southern California , Los Angeles , California , United States )
- Edegran, Albin ( Lund University , Malmö , Sweden )
- Fenton, Kathleen ( NATIONAL HEART LUNG AND BLOOD INST , Bethesda , Maryland , United States )
- Patel, Nirav ( Lenox Hill Hospital/Northwell Health , New York , New York , United States )
- Taddei-peters, Wendy ( NATL HEART LUNG AND BLOOD INST , Bethesda , Maryland , United States )
- Moskowitz, Alan ( Icahn School of Medicine at Mount Sinai , New York , New York , United States )
- Ogara, Patrick ( BRIGHAM AND WOMENS HOSPITAL , Boston , Massachusetts , United States )
- Gelijns, Annetine ( Icahn School of Medicine-Mt Sinai , New York , New York , United States )
- Alexander, John ( Duke University Medical Center , Durham , North Carolina , United States )
- Gillinov, A ( CLEVELAND CLINIC , Cleveland , Ohio , United States )
- Bagiella, Emilia ( Icahn School of Medicine at Mount S , New York , New York , United States )
- D'alessandro, David ( Massacusetts General Hospital , Boston , Massachusetts , United States )
- Dimaio, John ( , Dallas , Texas , United States )
- Bhavnani, Sanjeev ( Scripps Clinic , La Jolla , California , United States )
- Badhwar, Vinay ( West Virginia University , Morgantown , West Virginia , United States )
- Sengupta, Partho ( Rutgers RWJ Medical School , New Brunswick , New Jersey , United States )
- Johnson, Linda ( Lund University , Malmö , Sweden )
- Gajewska-dendek, Elzbieta ( Medicalgorithmics S.A , Warsaw , Poland )
Meeting Info:
Session Info:
Pushing the Boundaries: Innovations in Electrophysiology
Monday, 11/18/2024 , 11:10AM - 12:25PM
Moderated Digital Poster Session
More abstracts on this topic:
Damarlapally Nanush, Vempati Roopeessh, Vasudevan Srivatsa Surya, Banda Prathibha, Mathur Gaurav, Khan Afrasayab, Mourad Denise, Polamarasetty Harshavardhan, Desai Rupak
A Comparative Analysis of Esophageal Cooling for Preventing Esophageal Injury Post Atrial Fibrillation Catheter Ablation: A Systematic Review and Meta-analysisIbrahim Momen Mohamed, Al Hennawi Hussam, Tanas Yousef, Abourady Youmna, Sewedan Nourhan, Hashem Ahmed Magdy, Motawea Karam R.
More abstracts from these authors:
Alabbadi Sundos, Makkar Raj, Bagiella Emilia, Akowuah Enoch, Deshpande Ranjit, Bleiziffer Sabine, Bandettini W. Patricia, Akhter Shahab, Ogara Patrick, Iribarne Alexander, Egorova Natalia, Rodes-cabau Josep, Gelijns Annetine, Moskowitz Alan, Doenst Torsten, Chikwe Joanna, Toyoda Nana, Itagaki Shinobu, Krane Prof. Dr. Med. Markus
Mitral Valve Surgery in Arrhythmogenic Mitral Regurgitation: Special ConsiderationsBorger Michael, Adams David, Gillinov A Marc, Nguyen Tom, Ramzy Danny