Final ID: MDP1788
A novel approach for LV delay evaluation: non-invasive QLV measurement using UHF ECG
Abstract Body (Do not enter title and authors here): Introduction: Cardiac resynchronization therapy (CRT) improves quality of life, left ventricular (LV) systolic function and reduces heart failure hospitalizations and mortality. LV pacing at sites with prolonged electrical delay, such as invasively measured LV delay (QLV), is most effective in correcting electrical dyssynchrony in patients with LBBB-type intraventricular conduction abnormalities. UHF-ECG is a non-invasive tool optimized to calculate ventricular dyssynchrony between segments under the standard V1–V8 chest leads. However, the association between LV delay assessed by UHF-ECG and invasively assessed LV delay is still unknown. Our study aimed to compare invasive measurements of LV delay with LV delay using UHF ECG in patients with LBBB and undergoing CRT.
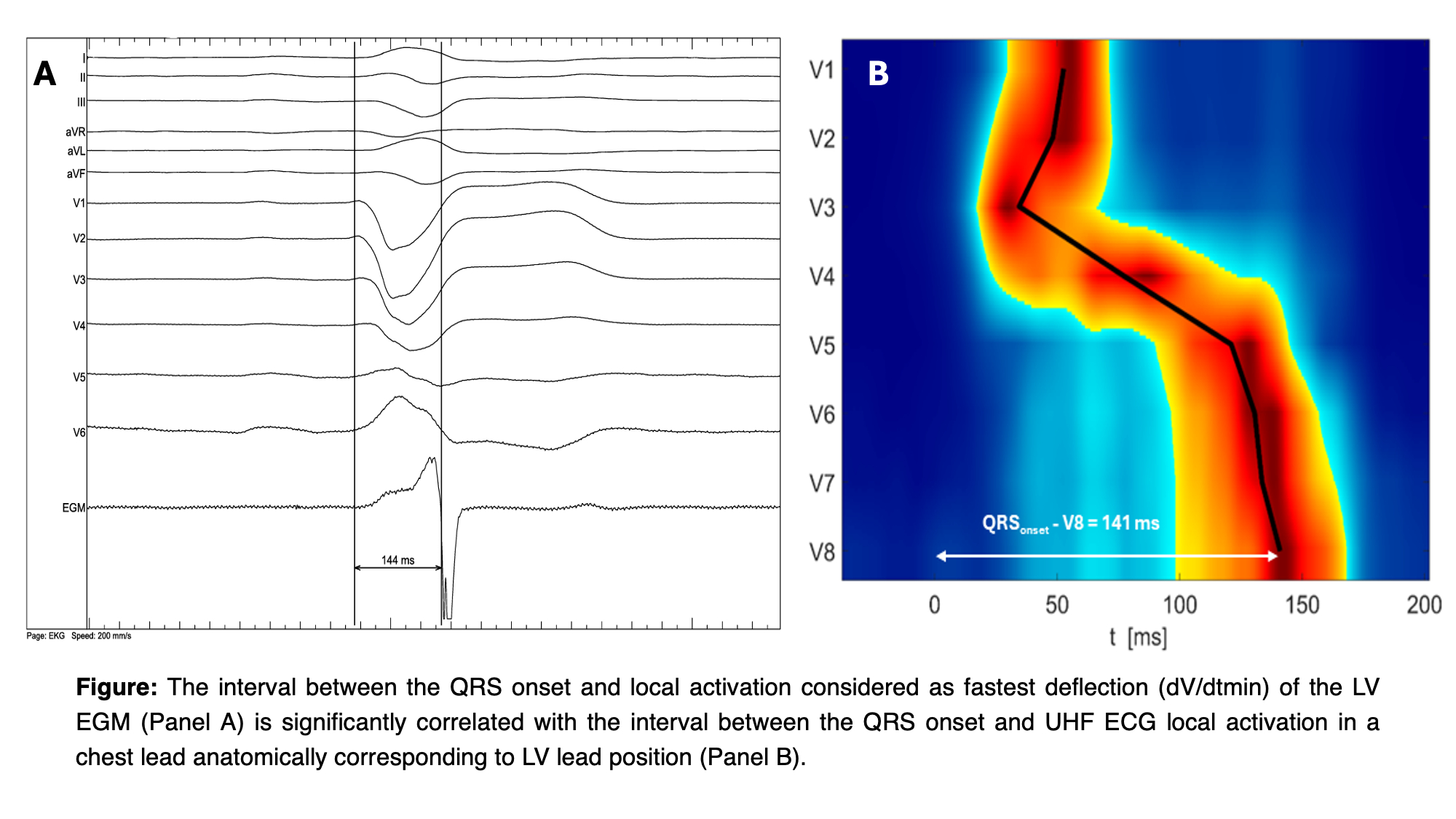
Methods: We retrospectively analyzed electrophysiologic recordings, angiographic images, and UHF-ECG recordings from consecutive BVP-CRT procedures. The study included patients with symptomatic heart failure with LVEF ≤ 40 %, QRS duration ≥ 130 ms and spontaneous sinus rhythm with a non-RBBB morphology. The QLV interval was measured from the QRS complex onset to the steepest deflection of the local electrogram from the implanted CS lead. To quantify LV delay using UHF ECG, the time from the QRS onset to the activations in V6, V7, and V8 was measured. The left ventricular lateral wall was segmented into two regions: the basal segment (activating under V7-V8 leads) and the apical segment (activating under the V6 lead). Each LV lead electrode was assigned to a segment based on angiographic images.
Results: Our study included 32 patients with an average LVEF of 30 ± 6 %, ischemic cardiomyopathy had 12 and Strauss criteria for LBBB met 28 patients. The average intrinsic QRSd was 171 ± 16 ms and spontanous e-dys was 82 ± 32 ms. There was no statistically significant difference between measured QLV and LV delay using UHF ECG (4.0 ± 8.4 ms; mean ± SD, p = 0.48) and linear regression analysis showed strong correlation between them (r = 0.95). Also, there was no difference in measurements between the apical and basal segments (3.3 ± 8.3 ms; mean ± SD, r = 0.95 for basal segment, r = 0.94 for apical segment, p = 0.14).
Conclusions: Our study demonstrated that UHF-ECG measurements of LV activation delay are strongly correlated with invasively measured electrical LV delay in patients with LBBB undergoing CRT. This suggests that UHF-ECG can accurately identify sites of prolonged electrical delay.
Methods: We retrospectively analyzed electrophysiologic recordings, angiographic images, and UHF-ECG recordings from consecutive BVP-CRT procedures. The study included patients with symptomatic heart failure with LVEF ≤ 40 %, QRS duration ≥ 130 ms and spontaneous sinus rhythm with a non-RBBB morphology. The QLV interval was measured from the QRS complex onset to the steepest deflection of the local electrogram from the implanted CS lead. To quantify LV delay using UHF ECG, the time from the QRS onset to the activations in V6, V7, and V8 was measured. The left ventricular lateral wall was segmented into two regions: the basal segment (activating under V7-V8 leads) and the apical segment (activating under the V6 lead). Each LV lead electrode was assigned to a segment based on angiographic images.
Results: Our study included 32 patients with an average LVEF of 30 ± 6 %, ischemic cardiomyopathy had 12 and Strauss criteria for LBBB met 28 patients. The average intrinsic QRSd was 171 ± 16 ms and spontanous e-dys was 82 ± 32 ms. There was no statistically significant difference between measured QLV and LV delay using UHF ECG (4.0 ± 8.4 ms; mean ± SD, p = 0.48) and linear regression analysis showed strong correlation between them (r = 0.95). Also, there was no difference in measurements between the apical and basal segments (3.3 ± 8.3 ms; mean ± SD, r = 0.95 for basal segment, r = 0.94 for apical segment, p = 0.14).
Conclusions: Our study demonstrated that UHF-ECG measurements of LV activation delay are strongly correlated with invasively measured electrical LV delay in patients with LBBB undergoing CRT. This suggests that UHF-ECG can accurately identify sites of prolonged electrical delay.
More abstracts on this topic:
Correlation Between CRT Response and Patient-Reported Outcomes in Heart Failure with Reduced Ejection Fraction Patients
Paul Aritra, Demian Joe, Varma Niraj, Finet J. Emanuel, Kochar Arshneel, Bader Feras, Wazni Oussama, Tang Wilson, Rickard John
A Rare Case of Sequential Impella Mechanical Failures due to Infective Endocarditis VegetationsSawalski Cathryn, Seu Michelle, Darki Amir