Final ID: Mo4008
Bivalirudin Reduces Major Bleeding And Cardiovascular Mortality in MI patients Undergoing PCI Compared to Unfractionated Heparin.
Abstract Body (Do not enter title and authors here): Background
Antithrombotic regimens play a pivotal role in averting complications and ischemic incidents post-percutaneous coronary intervention (PCI) in MI (myocardial infarction) patients. Bivalirudin stands as a viable alternative to unfractionated heparin in this cohort, demonstrating the efficacy and safety profiles.
Aim
We aimed to compare the efficacy and safety of bivalirudin versus unfractionated heparin in post-percutaneous coronary intervention (PCI) in MI (myocardial infarction) patients.
Research Question
What is the efficacy and safety of Bivalirudin compared to unfractionated heparin in patients with MI undergoing PCI, specifically in terms of major bleeding, cardiovascular mortality, and other major adverse cardiovascular events?
Methods
We systematically searched PubMed, including MEDLINE, Embase, Cochrane Library, Google Scholar, ClinicalTrials.gov, and EBSCOhost/CINAHL, from January 1, 2000, through May 29, 2024, for randomized controlled trials (RCTs) that evaluated Bivalirudin versus unfractionated heparin and with a study population of patients with MI undergoing PCI. Data extraction was done using a spreadsheet, and data analysis was done using RevMan 5.4.1 for meta-analysis. The primary efficacy and safety endpoints were major bleeding, major cardiovascular events, cardiovascular mortality, all-cause mortality, myocardial infarction, stent thrombosis, and stroke.
Results
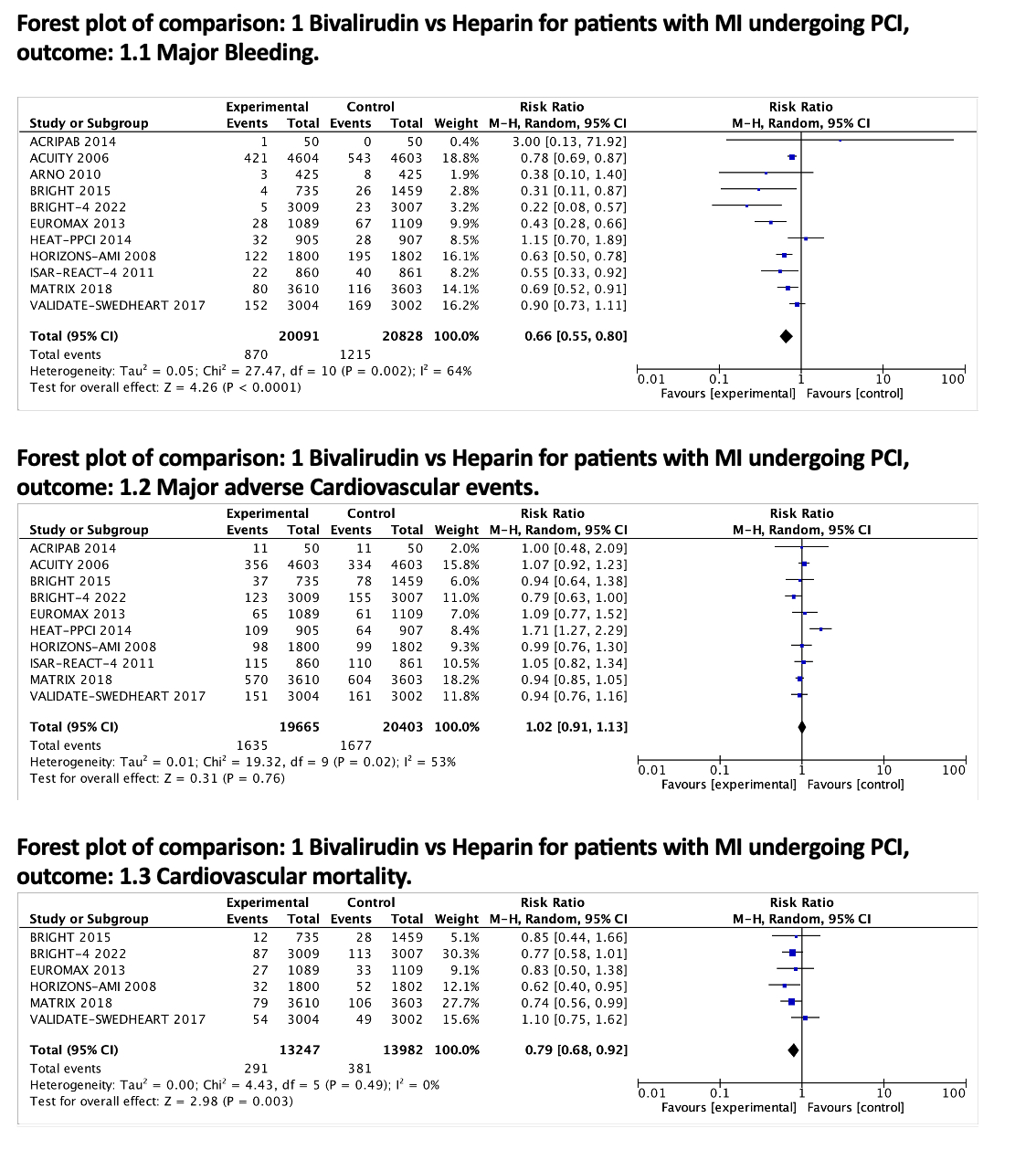
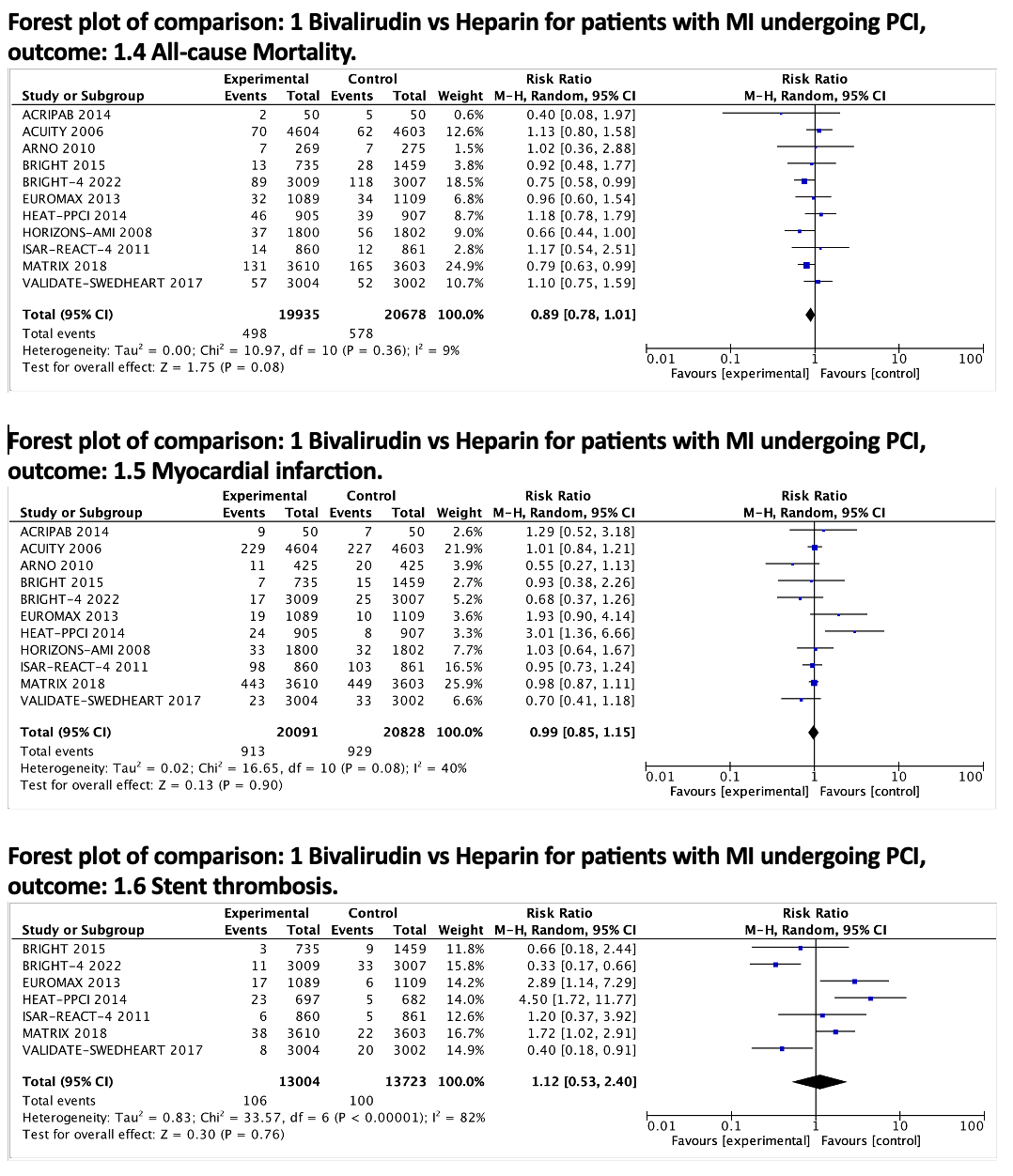
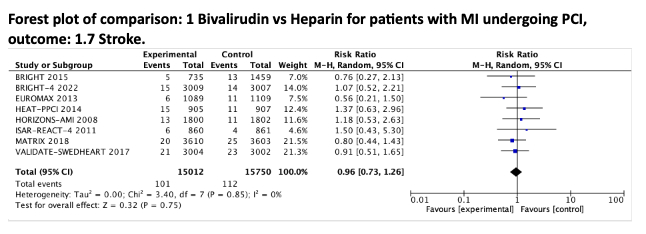
Our analysis included 11 RCTs, encompassing a total of 40,919 participants. When compared with unfractionated heparin, bivalirudin was associated with a significant reduction in major bleeding events (RR 0.66 [0.55 to 0.80]; p < 0.0001) and cardiovascular mortality (RR 0.79 [0.67 to 0.92]; p < 0.003). However, there were no significant differences between Bivalirudin and unfractionated heparin in terms of major adverse cardiovascular events (RR 1.02 [0.91 to 1.13]; p = 0.76), all-cause mortality (RR 0.89 [0.78 to 1.01]; p = 0.08), MI (RR 0.99 [0.85 to 1.15]; p = 0.90), stent thrombosis (RR 1.12 [0.53 to 2.40]; p = 0.76), or stroke (RR 0.96 [0.73 to 1.26]; p = 0.75).
Conclusion
Our meta-analysis indicates that in patients with MI undergoing PCI, Bivalirudin is associated with lower rates of major bleeding and cardiovascular mortality compared to unfractionated heparin. However, there were no significant differences observed in major adverse cardiovascular events, all-cause mortality, MI, stroke, or stent thrombosis between the two treatment groups.
Antithrombotic regimens play a pivotal role in averting complications and ischemic incidents post-percutaneous coronary intervention (PCI) in MI (myocardial infarction) patients. Bivalirudin stands as a viable alternative to unfractionated heparin in this cohort, demonstrating the efficacy and safety profiles.
Aim
We aimed to compare the efficacy and safety of bivalirudin versus unfractionated heparin in post-percutaneous coronary intervention (PCI) in MI (myocardial infarction) patients.
Research Question
What is the efficacy and safety of Bivalirudin compared to unfractionated heparin in patients with MI undergoing PCI, specifically in terms of major bleeding, cardiovascular mortality, and other major adverse cardiovascular events?
Methods
We systematically searched PubMed, including MEDLINE, Embase, Cochrane Library, Google Scholar, ClinicalTrials.gov, and EBSCOhost/CINAHL, from January 1, 2000, through May 29, 2024, for randomized controlled trials (RCTs) that evaluated Bivalirudin versus unfractionated heparin and with a study population of patients with MI undergoing PCI. Data extraction was done using a spreadsheet, and data analysis was done using RevMan 5.4.1 for meta-analysis. The primary efficacy and safety endpoints were major bleeding, major cardiovascular events, cardiovascular mortality, all-cause mortality, myocardial infarction, stent thrombosis, and stroke.
Results
Our analysis included 11 RCTs, encompassing a total of 40,919 participants. When compared with unfractionated heparin, bivalirudin was associated with a significant reduction in major bleeding events (RR 0.66 [0.55 to 0.80]; p < 0.0001) and cardiovascular mortality (RR 0.79 [0.67 to 0.92]; p < 0.003). However, there were no significant differences between Bivalirudin and unfractionated heparin in terms of major adverse cardiovascular events (RR 1.02 [0.91 to 1.13]; p = 0.76), all-cause mortality (RR 0.89 [0.78 to 1.01]; p = 0.08), MI (RR 0.99 [0.85 to 1.15]; p = 0.90), stent thrombosis (RR 1.12 [0.53 to 2.40]; p = 0.76), or stroke (RR 0.96 [0.73 to 1.26]; p = 0.75).
Conclusion
Our meta-analysis indicates that in patients with MI undergoing PCI, Bivalirudin is associated with lower rates of major bleeding and cardiovascular mortality compared to unfractionated heparin. However, there were no significant differences observed in major adverse cardiovascular events, all-cause mortality, MI, stroke, or stent thrombosis between the two treatment groups.
More abstracts on this topic:
Ability of Composite Magnetic Resonance Brain Imaging Scores to Predict Functional Outcomes in Survivors of Cardiac Arrest
Nguyen Thuhien, Town James, Wahlster Sarah, Johnson Nicholas, Poilvert Nicolas, Lin Victor, Ukatu Hope, Matin Nassim, Davis Arielle, Taylor Breana, Thomas Penelope, Sharma Monisha
A Machine Learning Readmission Risk Prediction Model for Cardiac DiseaseBailey Angela, Wang Wei, Shannon Clarence, Huling Jared, Tignanelli Christopher