Final ID: MDP245
The Impact of Vitamin D Status on Driveline Infections and Cerebral Vascular Accidents in Patients Undergoing Left Ventricular Assist Device Implantation
Abstract Body (Do not enter title and authors here): Introduction:
Left ventricular assist devices (LVADs) have become an increasingly common treatment option for patients with advanced heart failure, serving as either a bridge to transplantation or destination therapy. Despite major advancements in the field of mechanical circulatory support, cerebral vascular accidents (CVA) and driveline infections (DLI) continue to have a detrimental impact on morbidity and mortality.
Research Question:
Is there a higher incidence of DLI and CVA in vitamin D deficient patients that are undergoing LVAD implantation?
Goals/Aims:
We aimed to evaluate vitamin D deficiency as a potential risk factor for DLI and CVA in patients undergoing LVAD implantation.
Methods:
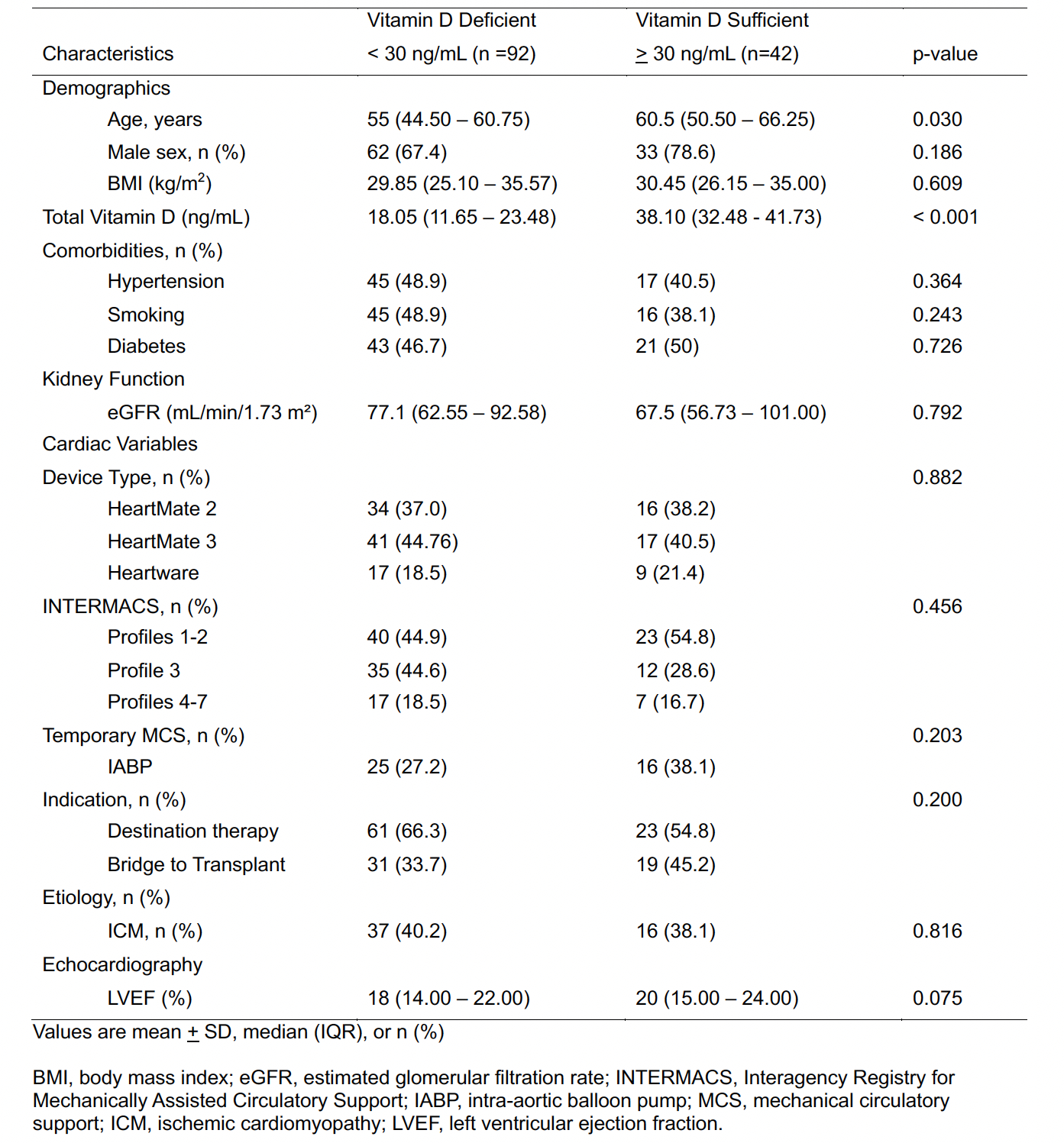
We performed a retrospective chart review of patients that underwent LVAD implantation at our institution from 2010 to 2022. Patients with vitamin D levels measured within 90 days of implantation were classified into either vitamin D sufficient (>30 ng/ml) or deficient (<30 ng/ml). The Kaplan-Meier method estimated 18-month freedom of DLI and CVA. The Cox proportional hazards model estimated the effect of deficiency on DLI/CVA risk. Baseline characteristics were recorded (table 1), and a multivariate cox model corrected for differences. Patients who were transplanted or expired were censored at their last clinic visit.
Results:
The study included 134 patients (mean age 53 +/- 13.23, 71.8% male), with 92 in the deficient group and 42 in the sufficient group. During the study period, 36 patients (27.5%) underwent transplant or expired, and there were 32 DLI and 7 CVA events. DLI-free survival was significantly higher in the sufficient group (90.5% vs. 69.6%, log rank p = 0.014). Patients in the sufficient group were found to be significantly older, but no other significant differences were found (Table 1). The unadjusted and age-adjusted hazard ratios for DLI were 3.430 (95% CI: 1.203 – 9.782, p = 0.021) and 3.190 (95% CI: 1.111 – 9.160, p = 0.031) respectively. No difference in CVA incidence was observed.
Conclusion:
Our findings support vitamin D deficiency as a potential modifiable risk factor for DLI, warranting further research to establish causality and assess the impact of vitamin D repletion on infection rates. Vitamin D levels did not appear to influence CVA incidence.
Left ventricular assist devices (LVADs) have become an increasingly common treatment option for patients with advanced heart failure, serving as either a bridge to transplantation or destination therapy. Despite major advancements in the field of mechanical circulatory support, cerebral vascular accidents (CVA) and driveline infections (DLI) continue to have a detrimental impact on morbidity and mortality.
Research Question:
Is there a higher incidence of DLI and CVA in vitamin D deficient patients that are undergoing LVAD implantation?
Goals/Aims:
We aimed to evaluate vitamin D deficiency as a potential risk factor for DLI and CVA in patients undergoing LVAD implantation.
Methods:
We performed a retrospective chart review of patients that underwent LVAD implantation at our institution from 2010 to 2022. Patients with vitamin D levels measured within 90 days of implantation were classified into either vitamin D sufficient (>30 ng/ml) or deficient (<30 ng/ml). The Kaplan-Meier method estimated 18-month freedom of DLI and CVA. The Cox proportional hazards model estimated the effect of deficiency on DLI/CVA risk. Baseline characteristics were recorded (table 1), and a multivariate cox model corrected for differences. Patients who were transplanted or expired were censored at their last clinic visit.
Results:
The study included 134 patients (mean age 53 +/- 13.23, 71.8% male), with 92 in the deficient group and 42 in the sufficient group. During the study period, 36 patients (27.5%) underwent transplant or expired, and there were 32 DLI and 7 CVA events. DLI-free survival was significantly higher in the sufficient group (90.5% vs. 69.6%, log rank p = 0.014). Patients in the sufficient group were found to be significantly older, but no other significant differences were found (Table 1). The unadjusted and age-adjusted hazard ratios for DLI were 3.430 (95% CI: 1.203 – 9.782, p = 0.021) and 3.190 (95% CI: 1.111 – 9.160, p = 0.031) respectively. No difference in CVA incidence was observed.
Conclusion:
Our findings support vitamin D deficiency as a potential modifiable risk factor for DLI, warranting further research to establish causality and assess the impact of vitamin D repletion on infection rates. Vitamin D levels did not appear to influence CVA incidence.
More abstracts on this topic:
Advanced Heart Failure and Mechanical Circulatory Support in the Context of Incarceration: A Clinical Challenge
Bhagat Siya, Ibecheozor Chukwukadibia, Sriwattanakomen Roy, Rhinehart Zachary, Hickey Gavin
β1-adrenergic autoantibodies (β1-AA) augment macropinocytosis in CD4+ T cells, leading to the expansion of CD4+CD28− T cell subsets in heart failure.Sun Fei, Yao Junyan, Li Bingjie, Zhang Suli, Liu Huirong