Final ID: 4144330
Long-term Prognosis of Historically Unrecognized Myocardial Infarction in Patients With Coronary Artery Disease
Abstract Body (Do not enter title and authors here):
Background
Clinically unrecognized myocardial infarction (MI) has been shown to have worse outcomes compared with the absence of MI in population-based studies of asymptomatic people and in symptomatic patients with suspected coronary artery disease (CAD) undergoing cardiac testing. Whether the adverse prognosis is due to the direct pathologic effects of MI or simply because it is a surrogate for CAD is unknown.
Methods
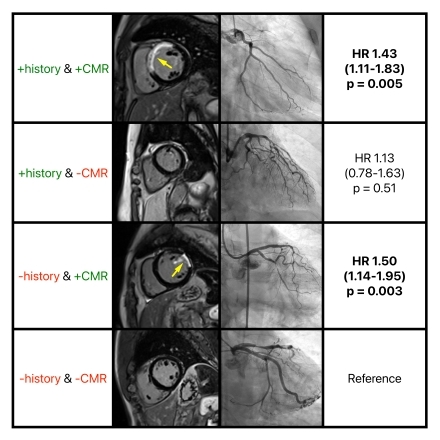
We conducted a retrospective cohort study of consecutive patients with established CAD who underwent clinical cardiovascular magnetic resonance imaging (CMR). A history of MI was established from documentation in their electronic medical records. MI on CMR was established based on ischemic late gadolinium enhancement. Patients were classified into four groups: 1) +history & +CMR, 2) +history & - CMR, 3) -history & +CMR, and 4) -history & -CMR. We investigated associations between these four groups and long-term death.
Results
Among 2,511 patients with CAD, 1,578 (63%) had MI by history (+history) and 1,914 (76%) had MI on CMR (+CMR). Overall, 1,362 (54%) had +history & +CMR, 216 (9%) had +history & -CMR, 552 (22%) had -history & +CMR, and 381 (15%) had -history & -CMR. During a median follow-up of 5.4 years (interquartile range 3.7, 8.1), 673 patients died. On Cox multivariable regression analyses adjusted to demographics, cardiac risk factors, comorbidities, and the extent of CAD, patients with -history & +CMR, and +history & + CMR had a greater risk of death [hazard ratio (HR) 1.50; 95% confidence interval (CI) 1.14-1.95; p=0.003 and HR 1.43; 95% CI 1.11-1.83; p=0.005 respectively) compared with patients with +history & -CMR and patients with -history & -CMR. Patients with +history & -CMR had no difference in mortality compared with patients with -history & -CMR (HR 1.13; 95% CI 0.78-1.63; p=0.51).
Conclusion
Among patients with CAD, those with -history & +CMR experience greater mortality, independent of the presence and extent of the underlying CAD. Conversely, patients with +history & -CMR have mortality rates comparable to those with -history & -CMR.
Background
Clinically unrecognized myocardial infarction (MI) has been shown to have worse outcomes compared with the absence of MI in population-based studies of asymptomatic people and in symptomatic patients with suspected coronary artery disease (CAD) undergoing cardiac testing. Whether the adverse prognosis is due to the direct pathologic effects of MI or simply because it is a surrogate for CAD is unknown.
Methods
We conducted a retrospective cohort study of consecutive patients with established CAD who underwent clinical cardiovascular magnetic resonance imaging (CMR). A history of MI was established from documentation in their electronic medical records. MI on CMR was established based on ischemic late gadolinium enhancement. Patients were classified into four groups: 1) +history & +CMR, 2) +history & - CMR, 3) -history & +CMR, and 4) -history & -CMR. We investigated associations between these four groups and long-term death.
Results
Among 2,511 patients with CAD, 1,578 (63%) had MI by history (+history) and 1,914 (76%) had MI on CMR (+CMR). Overall, 1,362 (54%) had +history & +CMR, 216 (9%) had +history & -CMR, 552 (22%) had -history & +CMR, and 381 (15%) had -history & -CMR. During a median follow-up of 5.4 years (interquartile range 3.7, 8.1), 673 patients died. On Cox multivariable regression analyses adjusted to demographics, cardiac risk factors, comorbidities, and the extent of CAD, patients with -history & +CMR, and +history & + CMR had a greater risk of death [hazard ratio (HR) 1.50; 95% confidence interval (CI) 1.14-1.95; p=0.003 and HR 1.43; 95% CI 1.11-1.83; p=0.005 respectively) compared with patients with +history & -CMR and patients with -history & -CMR. Patients with +history & -CMR had no difference in mortality compared with patients with -history & -CMR (HR 1.13; 95% CI 0.78-1.63; p=0.51).
Conclusion
Among patients with CAD, those with -history & +CMR experience greater mortality, independent of the presence and extent of the underlying CAD. Conversely, patients with +history & -CMR have mortality rates comparable to those with -history & -CMR.
More abstracts on this topic:
Advanced Cardiac MRI Parameters Phenomapping to Predict Outcomes in Patients with Nonischemic Cardiomyopathy
Ammoury Carl, Tang Wai Hong, Wang Xiaofeng, Kwon Deborah, Wu Yanjun, Korkerdsup Theerawat, Wang Tom Kai Ming, Rizkallah Diane, Bodi Kashyap, Calcagno Tess, Chen David, Nguyen Christopher
A Non-odorant Olfactory Receptor Ligand Depolymerizes the Platelet Actin Cytoskeleton to Prevent ThrombosisAggarwal Anu, Godwin Matthew, Ali Mariya, Jennings Courtney, Rajasekar Bhairavi, Scalise Alliefair, Stauffer Shaun, Mccrae Keith, Mcintyre Thomas, Cameron Scott, Wang Nancy, Josyula Vara Prasad, Yang Moua, Young Shim, Kennedy Quinn, Samuel Reina, Sangwan Naseer, Guntupalli Suman