Final ID: MDP285
Identifying the implementation potential for Mobile Integrated Health interventions for patients with heart failure
Abstract Body (Do not enter title and authors here): Introduction: Mobile Integrated Health (MIH) is a novel care delivery model utilizing community paramedics and telehealth to manage chronic illnesses such as heart failure (HF) outside hospital settings. Implementation of MIH is widely variable between institutions and stakeholder perspectives are poorly described in the literature.
Objective: To identify stakeholder (e.g., MIH experts, HF clinicians, and caregivers of adults with HF) perspectives on predisposing, enabling, and reinforcing factors to the adoption, implementation, and maintenance of MIH.
Methods: We used the RE-AIM (Reach Effectiveness Adoption Implementation Maintenance) framework to analyze MIH implementation. Stakeholders were recruited using a combination of convenience and snowball sampling nationally in the United States (U.S.). An interview guide based on the relevant domains of the RE-AIM framework was tailored to participant types. Interviews were conducted via phone or Zoom, with verbal consent obtained. Sessions were audio-recorded, transcribed verbatim, and qualitatively analyzed by four reviewers using directed content analysis.
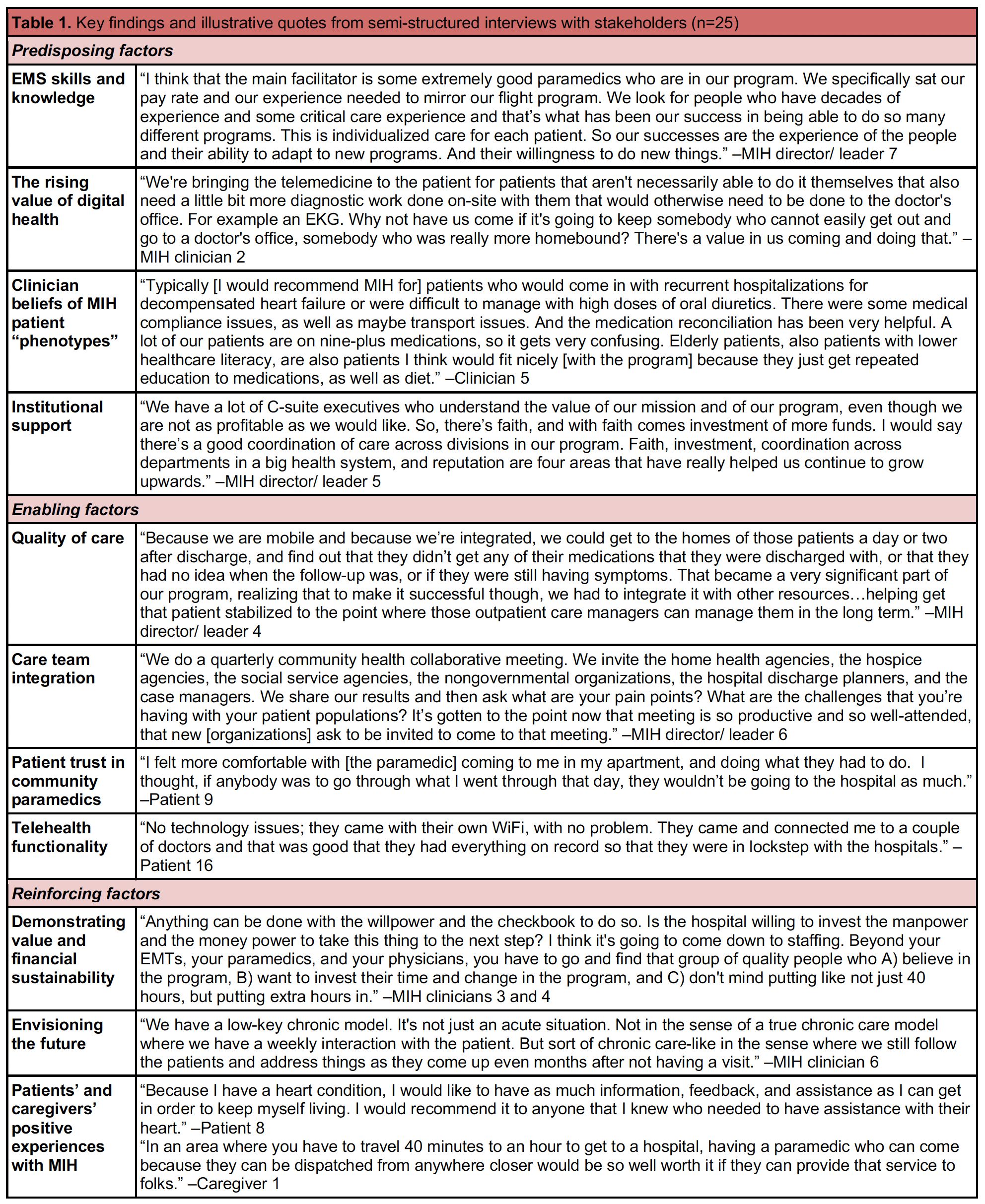
Results: Twenty-five stakeholders were recruited: six clinicians (four cardiologists, two nurses), eight MIH staff (four paramedics, one dispatcher, three nurse care coordinators), two caregivers, and nine MIH Program Directors. Predisposing factors included EMS skills and knowledge, the rising value of digital health, clinician beliefs about “phenotypes” of patients who benefit most from MIH, and alignment with the right outcome measures. Enabling factors included the comprehensiveness and quality of care provided during MIH visits, interdisciplinary team integration, patient trust in community paramedics, and telehealth functionality. Reinforcing factors included the ability of MIH programs to demonstrate value and financial sustainability, embrace future innovations and improvements, and show high patient satisfaction with MIH. Illustrative quotes are provided in Table 1.
Conclusions: This study highlighted unifying predisposing, enabling, and reinforcing factors across MIH programs nationally, which may guide future efforts for those launching or scaling these programs for adults with HF.
Objective: To identify stakeholder (e.g., MIH experts, HF clinicians, and caregivers of adults with HF) perspectives on predisposing, enabling, and reinforcing factors to the adoption, implementation, and maintenance of MIH.
Methods: We used the RE-AIM (Reach Effectiveness Adoption Implementation Maintenance) framework to analyze MIH implementation. Stakeholders were recruited using a combination of convenience and snowball sampling nationally in the United States (U.S.). An interview guide based on the relevant domains of the RE-AIM framework was tailored to participant types. Interviews were conducted via phone or Zoom, with verbal consent obtained. Sessions were audio-recorded, transcribed verbatim, and qualitatively analyzed by four reviewers using directed content analysis.
Results: Twenty-five stakeholders were recruited: six clinicians (four cardiologists, two nurses), eight MIH staff (four paramedics, one dispatcher, three nurse care coordinators), two caregivers, and nine MIH Program Directors. Predisposing factors included EMS skills and knowledge, the rising value of digital health, clinician beliefs about “phenotypes” of patients who benefit most from MIH, and alignment with the right outcome measures. Enabling factors included the comprehensiveness and quality of care provided during MIH visits, interdisciplinary team integration, patient trust in community paramedics, and telehealth functionality. Reinforcing factors included the ability of MIH programs to demonstrate value and financial sustainability, embrace future innovations and improvements, and show high patient satisfaction with MIH. Illustrative quotes are provided in Table 1.
Conclusions: This study highlighted unifying predisposing, enabling, and reinforcing factors across MIH programs nationally, which may guide future efforts for those launching or scaling these programs for adults with HF.
More abstracts on this topic:
A Multifaceted Blood Pressure Intervention Improves Medication Adherence in Low Income Adults with Hypertension
Krousel-wood Marie, Mitchell Tammy, Gray Winfrey Lea, Williams Shondra, Wiltz Gary, Winfrey Keith, Chen Jing, He Jiang, Peacock Erin, Mills Katherine, Allouch Farah, Cyprian Alecia, Davis Gerrelda, Fuqua Sonja, S Gilliam Darie, Greer Angel
A Bridge from Sweet to Sour: A Case of Recurrent Myocardial Stunning in Diabetic KetoacidosisSatish Vikyath, Pargaonkar Sumant, Slipczuk Leandro, Schenone Aldo, Maliha Maisha, Chi Kuan Yu, Sunil Kumar Sriram, Borkowski Pawel, Vyas Rhea, Rodriguez Szaszdi David Jose Javier, Kharawala Amrin, Seo Jiyoung