Final ID: Su2170
Effects of epicardial adipose tissue on cardiac function and exercise hemodynamics in patients with Heart Failure with Preserved Ejection Fraction
Abstract Body (Do not enter title and authors here): Background: Obesity is a risk factor for developing Heart Failure with Preserved Ejection Fraction (HFpEF). Epicardial adipose tissue (EAT), an ectopic fat depot located between the epicardium and the pericardium, has emerged as a potential risk factor for various cardiovascular diseases, including HFpEF. Previous studies have linked increased EAT thickness, measured by echocardiography, to elevated cardiac filling pressures and systolic and diastolic dysfunction. Compared to echo, a volumetric assessment of EAT with MRI has greater accuracy, precision, and reproducibility. This study aimed to assess the relationship between EAT and cardiac function and exercise hemodynamics in patients with HFpEF.
Methods: We studied 32 patients with HFpEF (19 women; BMI, 37±6kg/m2; age, 69±6years). Total and visceral fat were assessed with dual-energy x-ray absorptiometry. MRI was used to quantify EAT volume across short-axis slices and assess global longitudinal strain(GLS). We assessed ventricular filling pressures (right heart catheterization), oxygen uptake (VO2), cardiac output (Qc, Direct Fick), and diastolic function (echocardiography) on a seated upright cycle ergometer at rest, 20 Watts, and peak exercise (87±35 Watts). Correlation analyses were performed to examine the relationship between variables.
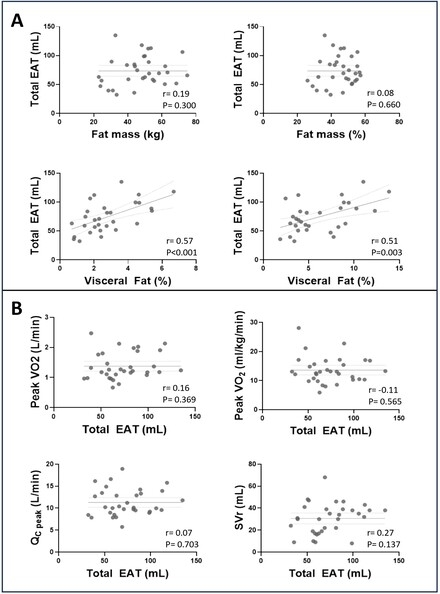
Results: EAT was moderately correlated with visceral adiposity (r=0.57, P<0.001) but not with total body fat (Figure, Panel A). EAT was not associated with markers of diastolic function (early tissue Doppler relaxation velocity [e'], mitral inflow velocity ratio [E/A], early mitral inflow/e' ratio [E/e']), cardiac filling pressures (right atrial pressure and pulmonary capillary wedge pressure) or mean pulmonary artery pressure at rest or during exercise. In addition, there was no association between GLS and total EAT (r=-0.06, P=0.735) or EAT located over the left ventricle (r=-0.05, P=0.749). EAT was not associated with exercise capacity (Figure, Panel B).
Conclusions: In patients with HFpEF, total EAT volume quantified with MRI did not correlate with measures of cardiac function at rest or during exercise. Our results suggest ventricular EAT does not impact cardiac function directly in patients with obesity and HFpEF.
Methods: We studied 32 patients with HFpEF (19 women; BMI, 37±6kg/m2; age, 69±6years). Total and visceral fat were assessed with dual-energy x-ray absorptiometry. MRI was used to quantify EAT volume across short-axis slices and assess global longitudinal strain(GLS). We assessed ventricular filling pressures (right heart catheterization), oxygen uptake (VO2), cardiac output (Qc, Direct Fick), and diastolic function (echocardiography) on a seated upright cycle ergometer at rest, 20 Watts, and peak exercise (87±35 Watts). Correlation analyses were performed to examine the relationship between variables.
Results: EAT was moderately correlated with visceral adiposity (r=0.57, P<0.001) but not with total body fat (Figure, Panel A). EAT was not associated with markers of diastolic function (early tissue Doppler relaxation velocity [e'], mitral inflow velocity ratio [E/A], early mitral inflow/e' ratio [E/e']), cardiac filling pressures (right atrial pressure and pulmonary capillary wedge pressure) or mean pulmonary artery pressure at rest or during exercise. In addition, there was no association between GLS and total EAT (r=-0.06, P=0.735) or EAT located over the left ventricle (r=-0.05, P=0.749). EAT was not associated with exercise capacity (Figure, Panel B).
Conclusions: In patients with HFpEF, total EAT volume quantified with MRI did not correlate with measures of cardiac function at rest or during exercise. Our results suggest ventricular EAT does not impact cardiac function directly in patients with obesity and HFpEF.
More abstracts on this topic:
Adipose tissue plasticity in response to early pathological stress on the heart and mediation by adipose thermogenic activation
James Natasha Maria, Stanford Kristin, Challa Azariyas, Vidal Souza Pablo, Pardeshi Parth, Maurya Santosh, Wang Yang, Baer Lisa, Carley Andrew, Lewandowski E Douglas
4D Flow MRI Allows for Enhanced Characterization of Aortic RegurgitationAvgousti Harris, Johnson Ethan, Berhane Haben, Thomas James, Allen Bradley, Markl Michael, Appadurai Vinesh