Final ID: MDP306
Factors Associated With Increased Inpatient Mortality Risk In End Stage Heart Failure Patients That May Help Providers To Identify triggers For Palliative Care Consultation
Abstract Body (Do not enter title and authors here): Introduction: Palliative care interventions for patients with heart failure have been shown to significantly improve quality of life, reduce symptom burden, and enhance functional status. Timing of referral becomes challenging as disease progresses and readmission rates increase. We studied factors associated with inpatient mortality in patients with end stage heart failure, ineligible for additional advanced therapies.
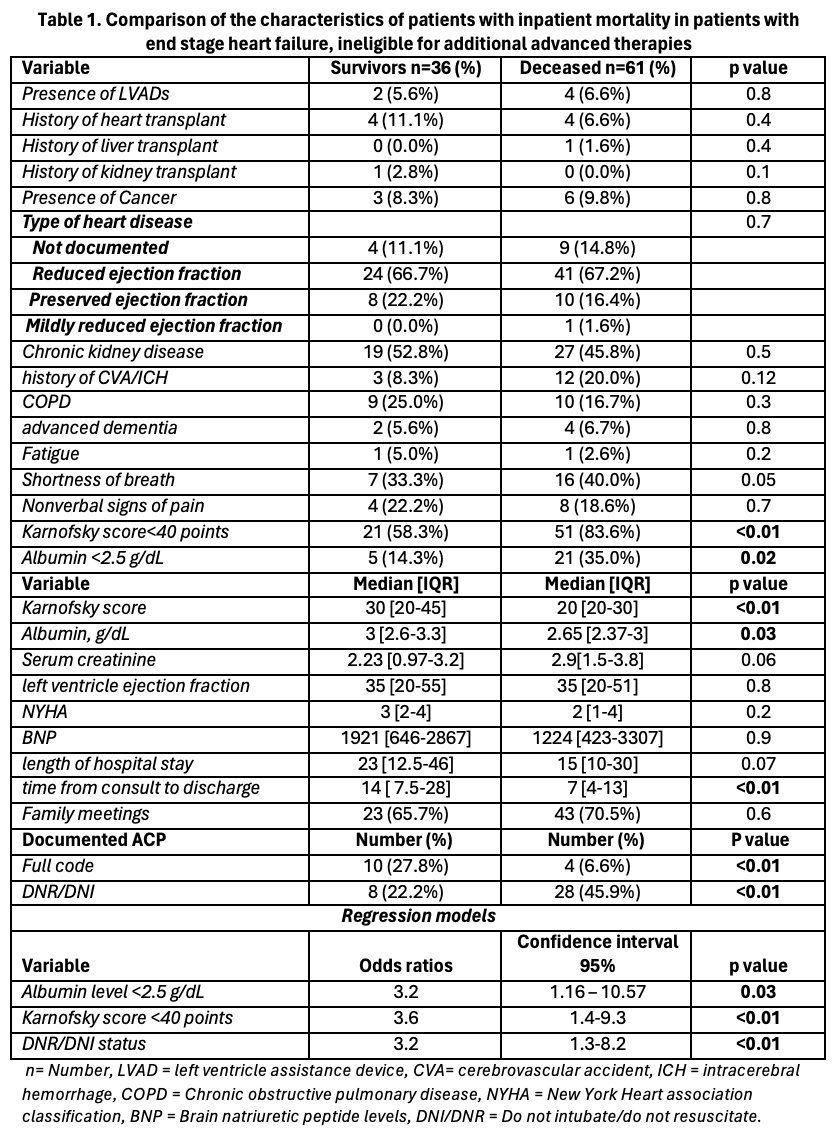
Methods: Individuals with acute decompensated heart failure admitted between 2021-2023, who were ineligible for further advanced cardiac therapies and referred to palliative care, were included to this retrospective study. Data on demographic variables, clinical parameters (NYHA classification, Karnofsky Performance Scale (KPS) scores, comorbidities, type of heart disease, BNP, albumin, creatinine levels), and palliative care interventions (symptom burden assessments, family meetings, and advanced care planning (ACP) discussions) were collected. We conducted bivariate and multivariate analyses using Kruskal-Wallis and chi-square tests, and adjusted regression models to compare characteristics between individuals who died while admitted and survivors.
Results: A total of 97 individuals were included in the study, with a mean age of 68 ± 17.7 years, 33.0%(n=32) of whom were female. Patients who died during admission had significantly higher rate of established ACP following palliative care consult (p< 0.01) and had a shorter time from consultation to discharge and were more likely to be declared DNR/DNI during admission. Hospital length of stay was shorter for patients who died in the hospital Lower KPS scores, with KPS scores <40 associated with increased hospital mortality (OR = 3.6 [CI 1.16–10.57], p < 0.01). Albumin levels were lower in this group, and levels <2.5 g/dL were associated with increased mortality (OR = 3.2 [CI 1.4–9.3], p < 0.01).
Conclusions: individuals with end-stage heart failure who have lower KPS scores, and reduced albumin levels may face a higher risk of in-hospital mortality and rapid disease progression. Identifying triggers such as severe symptom burden, complex decision-making needs, and functional decline can ensure timely and appropriate palliative care referrals.
Methods: Individuals with acute decompensated heart failure admitted between 2021-2023, who were ineligible for further advanced cardiac therapies and referred to palliative care, were included to this retrospective study. Data on demographic variables, clinical parameters (NYHA classification, Karnofsky Performance Scale (KPS) scores, comorbidities, type of heart disease, BNP, albumin, creatinine levels), and palliative care interventions (symptom burden assessments, family meetings, and advanced care planning (ACP) discussions) were collected. We conducted bivariate and multivariate analyses using Kruskal-Wallis and chi-square tests, and adjusted regression models to compare characteristics between individuals who died while admitted and survivors.
Results: A total of 97 individuals were included in the study, with a mean age of 68 ± 17.7 years, 33.0%(n=32) of whom were female. Patients who died during admission had significantly higher rate of established ACP following palliative care consult (p< 0.01) and had a shorter time from consultation to discharge and were more likely to be declared DNR/DNI during admission. Hospital length of stay was shorter for patients who died in the hospital Lower KPS scores, with KPS scores <40 associated with increased hospital mortality (OR = 3.6 [CI 1.16–10.57], p < 0.01). Albumin levels were lower in this group, and levels <2.5 g/dL were associated with increased mortality (OR = 3.2 [CI 1.4–9.3], p < 0.01).
Conclusions: individuals with end-stage heart failure who have lower KPS scores, and reduced albumin levels may face a higher risk of in-hospital mortality and rapid disease progression. Identifying triggers such as severe symptom burden, complex decision-making needs, and functional decline can ensure timely and appropriate palliative care referrals.
More abstracts on this topic:
Ambulatory Inotropic Support in Patients with Stage D Heart Failure Does Not Increase ICD Therapies
Sunthankar Kathryn, Pfaff Jamie, Farber-eger Eric, Richardson Travis, Wells Quinn, Ooi Henry, Skelton Melanie, Stevenson Lynne, Pedrotty Dawn
Outcomes of Heart Failure in Muscular Dystrophies in Adults: A Nationwide Analysis in the United StatesAbdul Jabbar Ali Bin, Al-salahat Ali, Dilsaver Danielle B., Ismayl Mahmoud, Goldsweig Andrew, Aboeata Ahmed