Final ID: MDP1229
Real-World Data On Cardiovascular Outcomes In Colchicine Use After Acute Myocardial Infarction
Abstract Body (Do not enter title and authors here): Background
After acute myocardial infarction (AMI), physicians typically address traditional coronary artery disease risk factors such as LDL-C, smoking, hypertension, and diabetes. However, residual inflammatory risk may be overlooked. Low-dose colchicine has been shown to reduce stroke and recurrent angina requiring revascularization in clinical trials, but real-world data is limited. This study aims to evaluate the use of colchicine post-AMI and its impact on cardiovascular outcomes.
Methods
We utilized the TriNetX database (January 2006 to January 2023) to include all new AMI patients aged ≥18 years who underwent revascularization, comparing those started on colchicine post-AMI to those who were not. Baseline characteristics were assessed. At a 5-year follow-up, outcomes such as death, cardiac arrest, recurrent AMI or revascularization, heart failure (HF), stroke, new-onset atrial fibrillation (AF), and diarrhea were evaluated.
Results
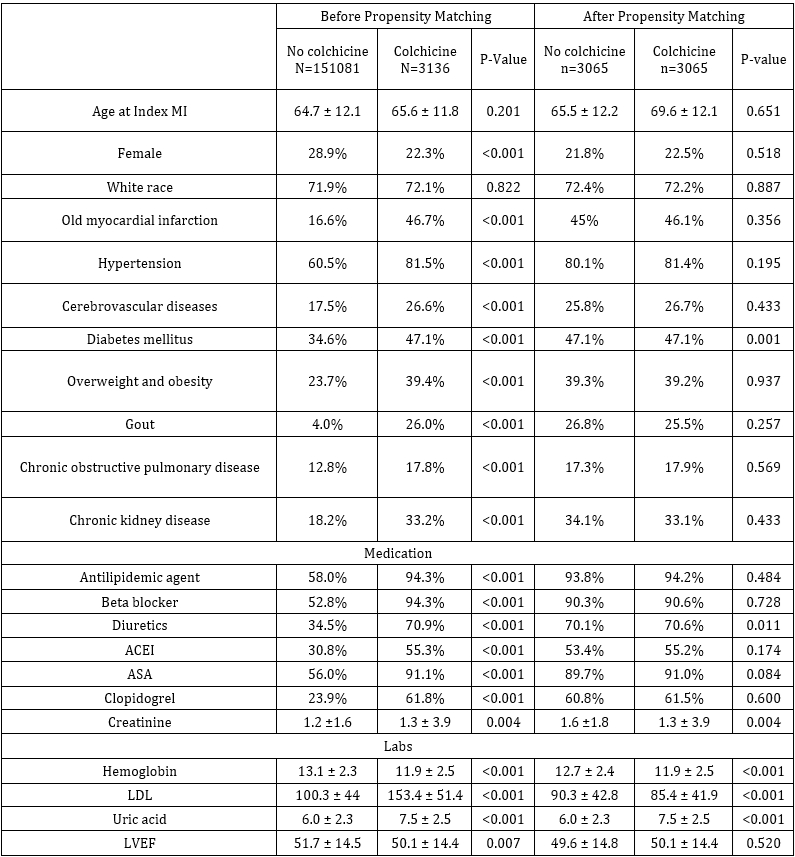
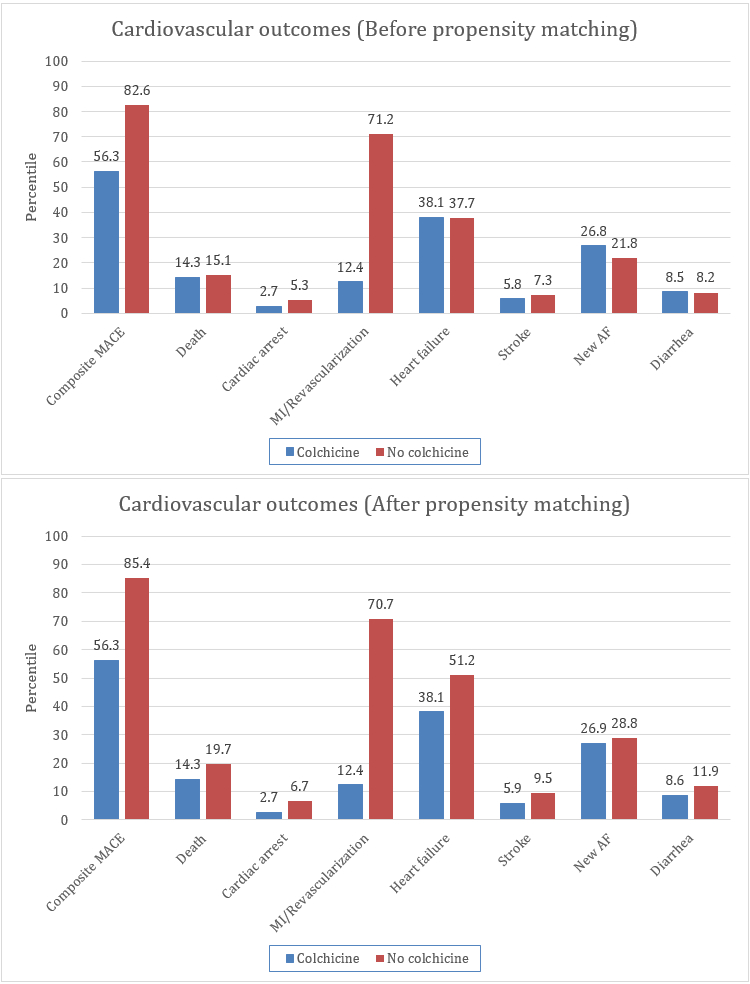
Out of 151,182 patients, 3,099 (2%) were started on colchicine after the index AMI. The mean ages were 64.7±12.1 years for the non-colchicine group and 65.6±11.8 years for the colchicine group. At 5 years, the colchicine group had a lower incidence of composite cardiovascular outcomes (56.3% vs. 82.6%, p < 0.01). Specifically, recurrent AMI/revascularization (12.4% vs. 71.2%, p <0.01), cardiac arrest (2.7% vs. 5.3%, p<0.01), and stroke (5.8% vs. 7.3%, p<0.01) were lower in the colchicine group. However, new-onset AF was higher in the colchicine group (26.8% vs. 21.8%, p<0.01). No significant differences were observed in death (14.3% vs. 15.1%, p=0.25), HF (38.1% vs. 37.7%, p=0.62), and diarrhea (8.5% vs. 8.2%, p=0.62). Propensity matching showed better cardiovascular outcomes for the colchicine group across all subgroups.
Conclusion
Colchicine use post-AMI is associated with improved cardiovascular outcomes in a real-world setting, although its utilization remains low.
After acute myocardial infarction (AMI), physicians typically address traditional coronary artery disease risk factors such as LDL-C, smoking, hypertension, and diabetes. However, residual inflammatory risk may be overlooked. Low-dose colchicine has been shown to reduce stroke and recurrent angina requiring revascularization in clinical trials, but real-world data is limited. This study aims to evaluate the use of colchicine post-AMI and its impact on cardiovascular outcomes.
Methods
We utilized the TriNetX database (January 2006 to January 2023) to include all new AMI patients aged ≥18 years who underwent revascularization, comparing those started on colchicine post-AMI to those who were not. Baseline characteristics were assessed. At a 5-year follow-up, outcomes such as death, cardiac arrest, recurrent AMI or revascularization, heart failure (HF), stroke, new-onset atrial fibrillation (AF), and diarrhea were evaluated.
Results
Out of 151,182 patients, 3,099 (2%) were started on colchicine after the index AMI. The mean ages were 64.7±12.1 years for the non-colchicine group and 65.6±11.8 years for the colchicine group. At 5 years, the colchicine group had a lower incidence of composite cardiovascular outcomes (56.3% vs. 82.6%, p < 0.01). Specifically, recurrent AMI/revascularization (12.4% vs. 71.2%, p <0.01), cardiac arrest (2.7% vs. 5.3%, p<0.01), and stroke (5.8% vs. 7.3%, p<0.01) were lower in the colchicine group. However, new-onset AF was higher in the colchicine group (26.8% vs. 21.8%, p<0.01). No significant differences were observed in death (14.3% vs. 15.1%, p=0.25), HF (38.1% vs. 37.7%, p=0.62), and diarrhea (8.5% vs. 8.2%, p=0.62). Propensity matching showed better cardiovascular outcomes for the colchicine group across all subgroups.
Conclusion
Colchicine use post-AMI is associated with improved cardiovascular outcomes in a real-world setting, although its utilization remains low.
More abstracts on this topic:
A Polypill Strategy for Lipid Lowering and Anti-Platelet Therapy After Acute Coronary Syndrome: A Pilot Randomized Controlled Trial
Keshvani Neil, Wang Thomas, Pandey Ambarish, Coellar Juan David, Rizvi Syed Kazim, Jain Anand, Bustillo-rubio M. Karina, Segar Matthew, Lokesh Nidhish, Miller James, Yates Sean
84 Immune checkpoint profiling in major aortic diseases leads to identification of potential roles of CD155-CD206 pathway in suppressing inflammation and immune responsesShao Ying, Saaoud Fatma, Xu Keman, Lu Yifan, Jiang Xiaohua, Wang Hong, Yang Xiaofeng