Final ID: Mo2035
Pediatric Paracorporeal VAD Antiplatelet Protocol
Abstract Body (Do not enter title and authors here): BACKGROUND: Ischemic stroke remains a dreaded complication of paracorporeal (continuous-PC; pulsatile-PP) ventricular assist devices (VADs) in pediatric patients. Advancements in anticoagulation management have improved the stroke rate to 12-17%, however, the management of antiplatelet therapy varies across centers. This study examines the outcomes of an antiplatelet protocol for patients with paracorporeal VADs at our center.
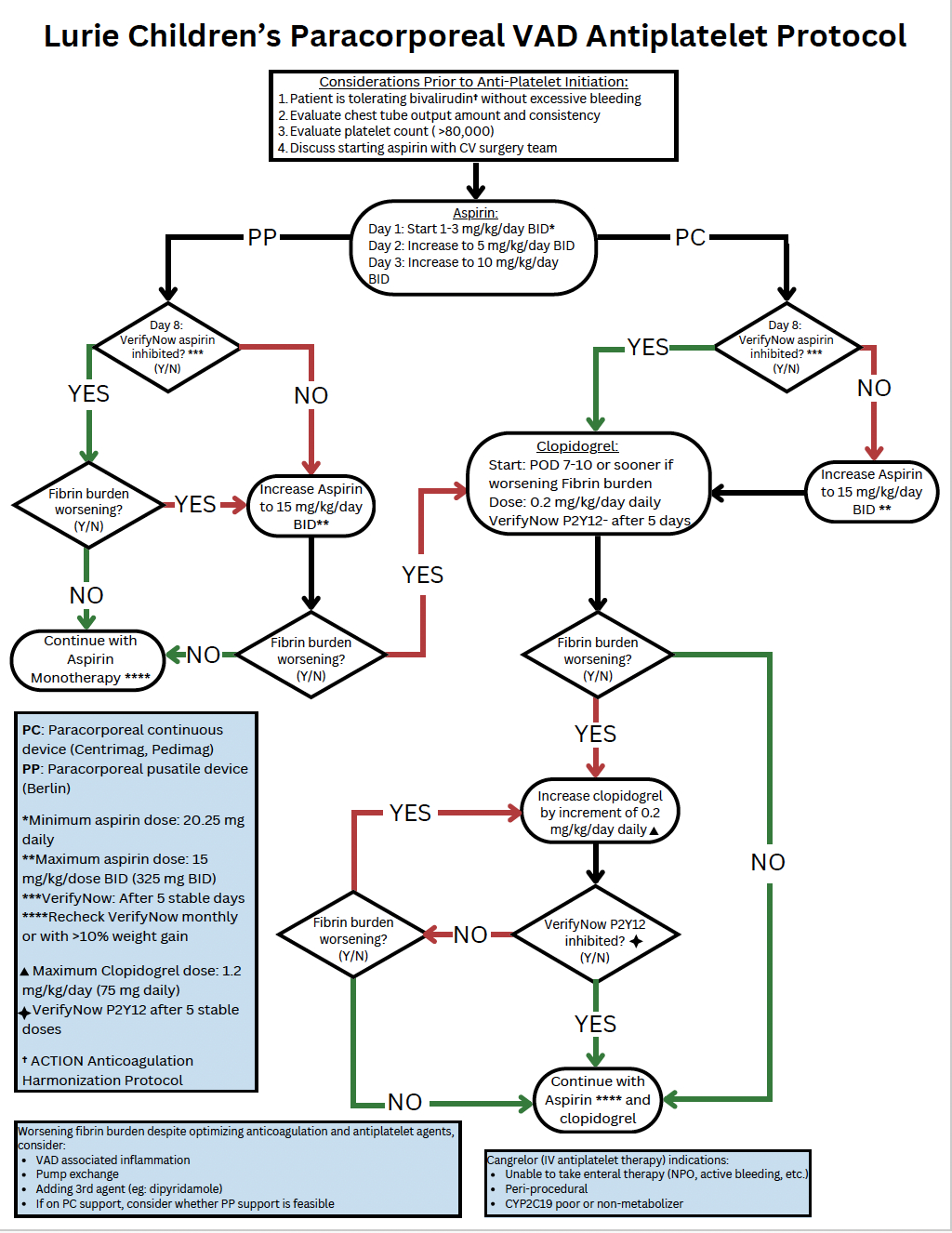
METHODS: We developed an antiplatelet protocol (Fig. 1) with dose adjustments guided by platelet function assays, VAD fibrin burden, and bleeding risk. We retrospectively reviewed patients with a paracorporeal VAD between December 2018 to December 2023. Demographic variables, incidence of thrombotic and bleeding events, and outcomes were assessed using descriptive statistics.
RESULTS: The cohort comprised 44 patients (52% male), median age 19 months (1 month - 8 years), with 22 (50%), 9 (20.5%), and 13 (29.5%) patients supported on PP, PC, and multiple VAD types respectively. Median support duration was 131 (PP; IQR 87, 183), 31 (PC; IQR 16, 46), and 88 (multiple VADs; IQR 66, 196) days. Diagnoses included cardiomyopathy 38% (n=17), congenital heart disease 57% (n=25) and others 5% (n=2). Thrombotic complications included: ischemic stroke in 6.8% (n=3) (1.9 events/100 patient months compared to 6-11 events/100 months reported in recent multicenter registry data); 11% (n=5) patients underwent 6 pump exchanges for fibrin burden. Major bleeding rate was 29.5% (n=13), most commonly gastrointestinal bleed; there were no hemorrhagic strokes. Five (11.3%) patients had an asymptomatic subdural hematoma (n=4 tiny/small, n=1 moderate). A positive clinical outcome was achieved in 86%, with 77% (n=34) bridged to transplant, 5% (n=2) explanted for recovery, and 5% (n=2) alive on device. Overall mortality was 14% (2 died on device, 4 transitioned to ECMO and died).
CONCLUSIONS: Our experience underscores the efficacy of a structured antiplatelet protocol in managing pediatric patients with paracorporeal VADs associated with a low stroke rate. Future studies are needed to assess the generalizability of these findings.
METHODS: We developed an antiplatelet protocol (Fig. 1) with dose adjustments guided by platelet function assays, VAD fibrin burden, and bleeding risk. We retrospectively reviewed patients with a paracorporeal VAD between December 2018 to December 2023. Demographic variables, incidence of thrombotic and bleeding events, and outcomes were assessed using descriptive statistics.
RESULTS: The cohort comprised 44 patients (52% male), median age 19 months (1 month - 8 years), with 22 (50%), 9 (20.5%), and 13 (29.5%) patients supported on PP, PC, and multiple VAD types respectively. Median support duration was 131 (PP; IQR 87, 183), 31 (PC; IQR 16, 46), and 88 (multiple VADs; IQR 66, 196) days. Diagnoses included cardiomyopathy 38% (n=17), congenital heart disease 57% (n=25) and others 5% (n=2). Thrombotic complications included: ischemic stroke in 6.8% (n=3) (1.9 events/100 patient months compared to 6-11 events/100 months reported in recent multicenter registry data); 11% (n=5) patients underwent 6 pump exchanges for fibrin burden. Major bleeding rate was 29.5% (n=13), most commonly gastrointestinal bleed; there were no hemorrhagic strokes. Five (11.3%) patients had an asymptomatic subdural hematoma (n=4 tiny/small, n=1 moderate). A positive clinical outcome was achieved in 86%, with 77% (n=34) bridged to transplant, 5% (n=2) explanted for recovery, and 5% (n=2) alive on device. Overall mortality was 14% (2 died on device, 4 transitioned to ECMO and died).
CONCLUSIONS: Our experience underscores the efficacy of a structured antiplatelet protocol in managing pediatric patients with paracorporeal VADs associated with a low stroke rate. Future studies are needed to assess the generalizability of these findings.
More abstracts on this topic:
Angiotensin Converting Enzyme Gene Polymorphisms (ACE-I/D) Do Not Predict Exercise-Induced Cardiac Remodeling or Performance in Adolescent Male Athletes
Becker Kristian, Hardie William, Gubanich Paul, Hill Garick, Logan Kelsey, Martin Lisa, Powell Adam
Antithrombotic trends before and after publication of randomized clinical trials in cervical artery dissection: A secondary analysis of the STOP-CAD StudyPenckofer Mary, Salehi Omran Setareh, Seiffge David, Arnold Marcel, Marialuisa Zedde, Zubair Adeel, Marto Joao Pedro, Ghannam Malik, Engelter Stefan, Traenka Christopher, Mac Grory Brian, Shu Liqi, Kam Wayneho, Elnazeir Marwa, Romoli Michele, Saleh Velez Faddi, Siegler James, Strelecky Lukas, Yaghi Shadi, Henninger Nils, Muppa Jayachandra, Bakradze Ekaterina, Heldner Mirjam, Katheryna Antonenko