Final ID: MDP953
Cell-free DNA Analysis Profiles End-Organ Injury and Predicts Outcomes with Left Ventricular Assist Device Implantation
Abstract Body (Do not enter title and authors here): Introduction
Durable left ventricular assist devices (LVADs) improve survival in heart failure but carry high risks of infection, hemocompatibility-related adverse events (HRAE), and death. Current clinical tools use subjective assessments or do not incorporate changes in end-organ injury, limiting their prognostic value with these complications. Plasma cell-free DNA (cfDNA), a potential marker for systemic and tissue-specific injury, holds promise to enhance patient risk stratification and prognosis.
Hypothesis
LVAD implantation decreases systemic and end-organ injury, measured by cfDNA.
Goal
We aimed to assess changes in global and organ-specific injury patterns with LVAD implantation via cfDNA, and to determine if pre-LVAD cfDNA levels predict post-LVAD complications.
Methods
We prospectively recruited 40 LVAD candidates and 40 healthy controls. Pre- and post-LVAD plasma samples were analyzed for nuclear cfDNA (ncfDNA) and mitochondrial cfDNA (mtcfDNA) using digital droplet PCR. Tissue-specific cfDNA levels were measured using bisulfite sequencing and a deconvolution algorithm with a DNA methylation library. Wilcoxon sign-rank tests were used to compare cfDNA levels, and log-rank tests were used to compare outcomes. The clinical outcomes were HRAE-free survival (major bleeding, stroke, device thrombosis, death), and post-LVAD infection. Random forest machine learning analysis ranked tissue-specific cfDNA to identify the tissue patterns of those who develop HRAE and those who develop infection.
Results
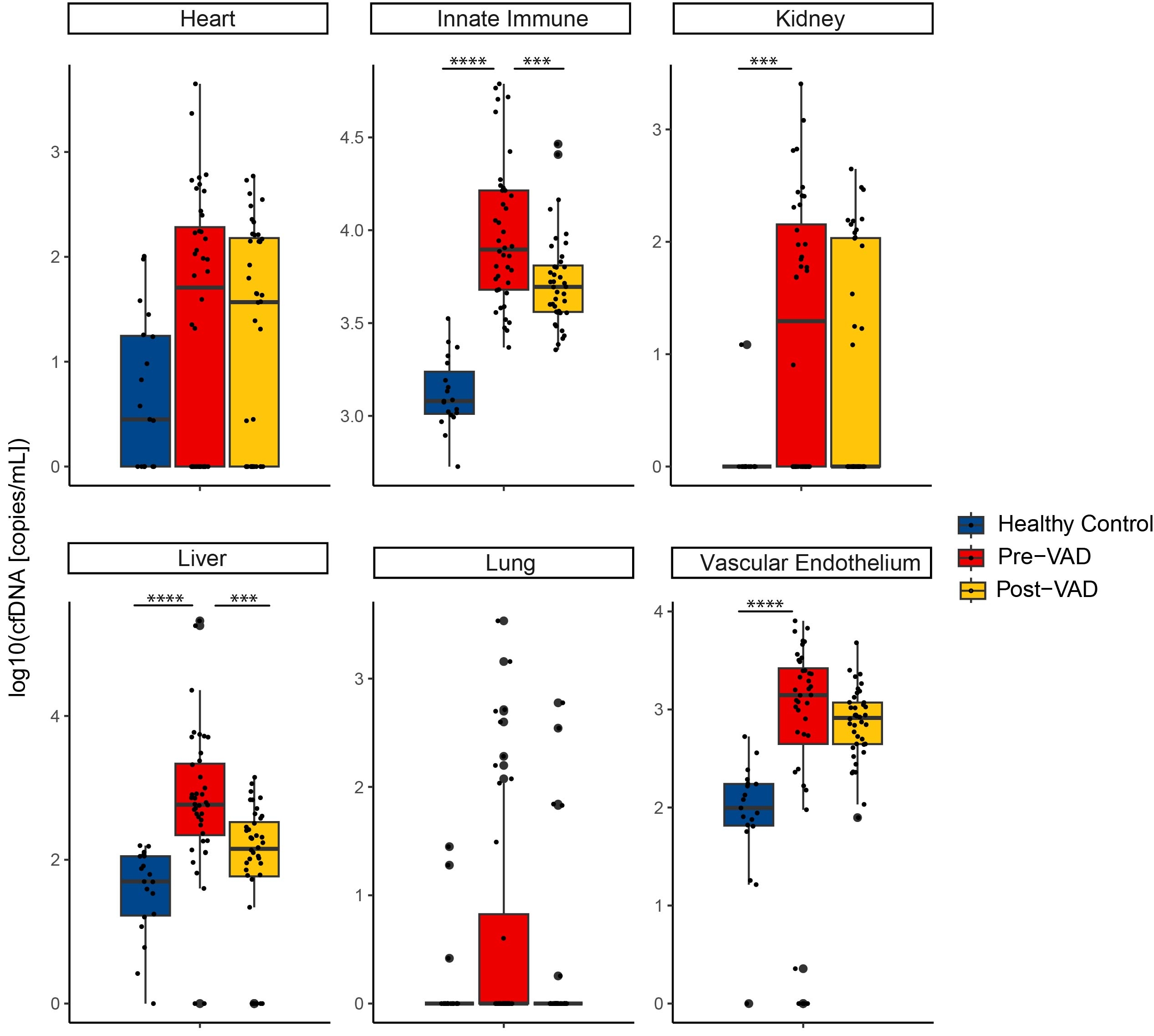
Prior to LVAD implantation, patients had 4-fold higher ncfDNA and 2-fold higher mtcfDNA compared to healthy controls. After LVAD placement, ncfDNA (18980 vs. 10228 copies/mL, p < .001) and mtcfDNA levels (1051882 vs 579609 copies/mL, p < .001) nearly halved, with significant reductions in innate immune and liver cfDNA (Figure). High pre-LVAD ncfDNA levels were associated with worse HRAE-free survival (p = .035) and infection (p < .001). Tissue sources important in determining HRAEs were distinct from those related to infections.
Conclusion
LVAD placement significantly improves systemic and tissue-specific injury, measured by reductions in cfDNA. While pre-LVAD cfDNA levels predict both post-LVAD HRAEs and infections, the cfDNA tissue contributions influencing these outcomes are distinct. Future studies will need to validate these findings and compare cfDNA to other predictors of poor LVAD outcomes.
Durable left ventricular assist devices (LVADs) improve survival in heart failure but carry high risks of infection, hemocompatibility-related adverse events (HRAE), and death. Current clinical tools use subjective assessments or do not incorporate changes in end-organ injury, limiting their prognostic value with these complications. Plasma cell-free DNA (cfDNA), a potential marker for systemic and tissue-specific injury, holds promise to enhance patient risk stratification and prognosis.
Hypothesis
LVAD implantation decreases systemic and end-organ injury, measured by cfDNA.
Goal
We aimed to assess changes in global and organ-specific injury patterns with LVAD implantation via cfDNA, and to determine if pre-LVAD cfDNA levels predict post-LVAD complications.
Methods
We prospectively recruited 40 LVAD candidates and 40 healthy controls. Pre- and post-LVAD plasma samples were analyzed for nuclear cfDNA (ncfDNA) and mitochondrial cfDNA (mtcfDNA) using digital droplet PCR. Tissue-specific cfDNA levels were measured using bisulfite sequencing and a deconvolution algorithm with a DNA methylation library. Wilcoxon sign-rank tests were used to compare cfDNA levels, and log-rank tests were used to compare outcomes. The clinical outcomes were HRAE-free survival (major bleeding, stroke, device thrombosis, death), and post-LVAD infection. Random forest machine learning analysis ranked tissue-specific cfDNA to identify the tissue patterns of those who develop HRAE and those who develop infection.
Results
Prior to LVAD implantation, patients had 4-fold higher ncfDNA and 2-fold higher mtcfDNA compared to healthy controls. After LVAD placement, ncfDNA (18980 vs. 10228 copies/mL, p < .001) and mtcfDNA levels (1051882 vs 579609 copies/mL, p < .001) nearly halved, with significant reductions in innate immune and liver cfDNA (Figure). High pre-LVAD ncfDNA levels were associated with worse HRAE-free survival (p = .035) and infection (p < .001). Tissue sources important in determining HRAEs were distinct from those related to infections.
Conclusion
LVAD placement significantly improves systemic and tissue-specific injury, measured by reductions in cfDNA. While pre-LVAD cfDNA levels predict both post-LVAD HRAEs and infections, the cfDNA tissue contributions influencing these outcomes are distinct. Future studies will need to validate these findings and compare cfDNA to other predictors of poor LVAD outcomes.
More abstracts on this topic:
A Novel Deep Learning Approach for Prediction of Right Heart Failure After Left Ventricular Assist Device Implantation using Pulmonary Artery Pressure Tracings
Lamicq Melissa, Buchanan Cole, Lateef Azalfa, Atteya Miriam, Houston Brian, Tedford Ryan, Wehbe Ramsey
A Genome-wide CRISPRi Screen Implicates Coronary Artery Disease GWAS Genes as Key Regulators of Adventitial Fibroblast ProliferationJackson William, Zhu Ashley, Gu Wenduo, Berezowitz Alexa, Iyer Meghana, Cheng Paul