Final ID: MDP422
Integrating Clinical, Genetic, and Electrocardiogram-Based Artificial Intelligence to Estimate Risk of Incident Atrial Fibrillation
Abstract Body (Do not enter title and authors here): Background: Atrial fibrillation (AF) risk estimation is feasible using clinical factors, inherited predisposition, and artificial intelligence (AI)-enabled electrocardiogram (ECG) analysis. Whether integrating these distinct risk signals improves AF risk estimation is unknown.
Methods: In the UK Biobank prospective cohort study, we estimated AF risk using three models derived from external populations: the well-validated Cohorts for Aging in Heart and Aging Research in Genomic Epidemiology AF (CHARGE-AF) clinical score, a published AI-enabled ECG-based AF risk model (ECG-AI), and a 1113667-variant AF polygenic risk score (PRS). We estimated discrimination of 5-year incident AF using time-dependent area under the receiver operating characteristic (AUROC) and average precision (AP).
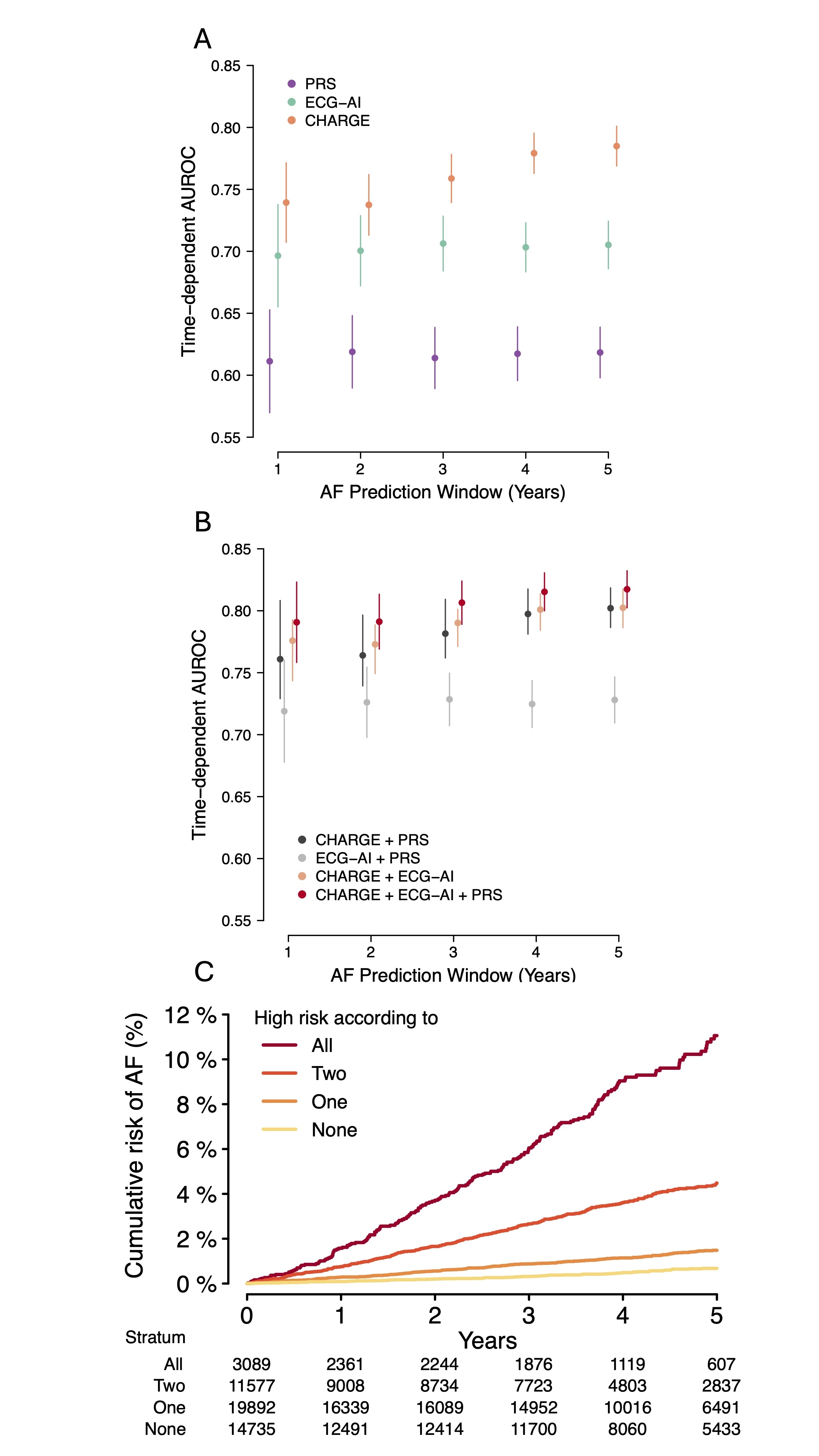
Results: Among 49,293 individuals (mean age 65±8 years, 52% women), 825 (2.4%) developed AF within 5 years. Using single models, discrimination of 5-year incident AF was higher using ECG-AI (AUROC 0.705 [95%CI 0.686-0.724]; AP 0.085 [0.071-0.11]) and CHARGE-AF (AUROC 0.785 [0.769-0.801]; AP 0.053 [0.048-0.061]) versus the PRS (AUROC 0.618, [0.598-0.639]; AP 0.038 [0.028-0.045]). The best performing two component model was CHARGE-AF+ECG-AI (AUROC 0.802 [0.786-0.818]; AP 0.098 [0.081-0.13]), with further improvement observed with inclusion of all components (“Total-AF”, AUROC 0.817 [0.802-0.832]; AP 0.11 [0.091-0.15], p<0.01 vs CHARGE-AF+ECG-AI). Using Total-AF, individuals at high AF risk (i.e., 5-year predicted AF risk >2.5%) had a 5-year cumulative incidence of AF of 5.83% (5.33-6.32). At the same threshold, the 5-year cumulative incidence of AF was progressively higher according to the number of models predicting high risk (zero: 0.67% [0.51-0.84], one: 1.48% [1.28-1.69], two: 4.48% [3.99-4.98]; three: 11.06% [9.48-12.61]. Total-AF achieved favorable net reclassification improvement compared to both CHARGE-AF+ECG-AI (0.039 [0.015-0.066]) and CHARGE-AF+PRS (0.033 [0.0082-0.059]).
Conclusions: Integration of clinical, genetic, and AI-derived risk signals improves discrimination of 5-year AF risk over individual components. Models such as Total-AF have potential to improve the prioritization of individuals for AF screening.
Methods: In the UK Biobank prospective cohort study, we estimated AF risk using three models derived from external populations: the well-validated Cohorts for Aging in Heart and Aging Research in Genomic Epidemiology AF (CHARGE-AF) clinical score, a published AI-enabled ECG-based AF risk model (ECG-AI), and a 1113667-variant AF polygenic risk score (PRS). We estimated discrimination of 5-year incident AF using time-dependent area under the receiver operating characteristic (AUROC) and average precision (AP).
Results: Among 49,293 individuals (mean age 65±8 years, 52% women), 825 (2.4%) developed AF within 5 years. Using single models, discrimination of 5-year incident AF was higher using ECG-AI (AUROC 0.705 [95%CI 0.686-0.724]; AP 0.085 [0.071-0.11]) and CHARGE-AF (AUROC 0.785 [0.769-0.801]; AP 0.053 [0.048-0.061]) versus the PRS (AUROC 0.618, [0.598-0.639]; AP 0.038 [0.028-0.045]). The best performing two component model was CHARGE-AF+ECG-AI (AUROC 0.802 [0.786-0.818]; AP 0.098 [0.081-0.13]), with further improvement observed with inclusion of all components (“Total-AF”, AUROC 0.817 [0.802-0.832]; AP 0.11 [0.091-0.15], p<0.01 vs CHARGE-AF+ECG-AI). Using Total-AF, individuals at high AF risk (i.e., 5-year predicted AF risk >2.5%) had a 5-year cumulative incidence of AF of 5.83% (5.33-6.32). At the same threshold, the 5-year cumulative incidence of AF was progressively higher according to the number of models predicting high risk (zero: 0.67% [0.51-0.84], one: 1.48% [1.28-1.69], two: 4.48% [3.99-4.98]; three: 11.06% [9.48-12.61]. Total-AF achieved favorable net reclassification improvement compared to both CHARGE-AF+ECG-AI (0.039 [0.015-0.066]) and CHARGE-AF+PRS (0.033 [0.0082-0.059]).
Conclusions: Integration of clinical, genetic, and AI-derived risk signals improves discrimination of 5-year AF risk over individual components. Models such as Total-AF have potential to improve the prioritization of individuals for AF screening.
More abstracts on this topic:
Combining Noncoding and Coding Genetic Variation Improves Arrhythmia Risk Prediction
Monroe Tanner, Pesce Lorenzo, Kearns Samuel, Page Patrick, Dellefave-castillo Lisa, Webster Gregory, Puckelwartz Megan, Mcnally Elizabeth
A novel risk score predicts the prevalence of left atrial low-voltage areas and rhythm outcome in patients undergoing long-standing persistent atrial fibrillation ablationOoka Hirotaka, Nakao Sho, Kusuda Masaya, Ariyasu Wataru, Kudo Satoshi, Fujii Subaru, Mano Toshiaki, Matsuda Yasuhiro, Masuda Masaharu, Okamoto Shin, Ishihara Takayuki, Nanto Kiyonori, Tsujimura Takuya, Hata Yosuke, Uematsu Hiroyuki