Final ID: Mo2019
Altered Pulmonary Arterial Hemodynamics in Repaired Tetralogy of Fallot Patients Referred for Pulmonary Valve Replacement: A Cross-Sectional 4D Flow Study
Abstract Body (Do not enter title and authors here): Background
Repaired tetralogy of Fallot (rTOF) patients require pulmonary valve replacement (PVR). Indexed right ventricular systolic/diastolic volumes are currently used to determine PVR timing, but there are recognized limitations. Unique hemodynamic features in the pulmonary arteries of these patients have been found using 4D flow cardiovascular magnetic resonance (CMR), which we hypothesize may inform PVR timing.
Hypothesis
Hemodynamic alterations in the pulmonary arteries of rTOF patients may inform timing of PVR.
Aims
To compare pulmonary arterial hemodynamics for rTOF patients who were/were not indicated for PVR after the exams using 4D flow CMR.
Methods
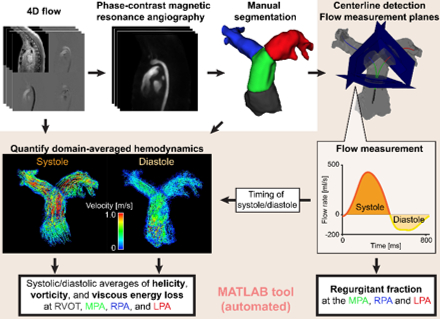
Clinical 4D flow CMR exams of rTOF patients were accessed retrospectively with IRB approval. Patients were classified into two groups depending on whether they underwent PVR after the CMR exam. Age-matched controls’ 4D flow data were also included. After pre-processing of 4D flow, the right ventricular outflow tract, main, left and right pulmonary arteries (RVOT, MPA, LPA and RPA) were manually segmented from phase-contrast magnetic resonance angiography. In addition to basic flow metrics such as regurgitant fraction, systolic and diastolic averages of helicity, vorticity, and viscous energy loss were computed for the four subdomains using an automated pipeline (Fig.1). Indexed end-systolic/diastolic right ventricular volumes were obtained from clinical CMR reports. P<0.05 was considered statistically significant.
Results
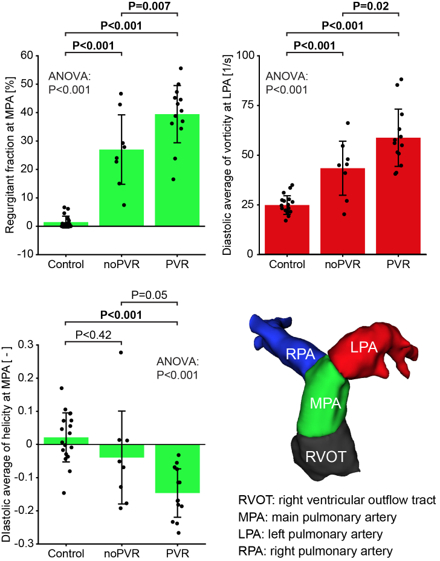
Eighteen controls (age, 14.9 [11.7-17.0] years) and 21 rTOF patients, consisting of 8 without PVR (noPVR; age, 14.7 [9.6-23.4] years) and 13 indicated for PVR after the exam (PVR; age, 16.1 [8.7 -20.3 years]; days between CMR and PVR, 134 [59.5 – 189.3] days), were included. The PVR group had significantly larger indexed right ventricular volume than the noPVR group (P=0.002; Table 1). Regurgitant fraction and diastolic vorticity at the LPA were significantly larger in the PVR group (P=0.007 for regurgitant fraction; P=0.02 for vorticity; Fig.2AB). Although not statistically significant, diastolic helicity at the MPA showed borderline significance (P=0.05; Fig.2C).
Conclusion
In addition to right ventricular dilatation and larger regurgitant fraction, patients indicated for PVR had larger vorticity in the LPA. This preliminary result could be used for future longitudinal study to determine hemodynamic markers that inform PVR timing. A larger cohort is under evaluation.
Repaired tetralogy of Fallot (rTOF) patients require pulmonary valve replacement (PVR). Indexed right ventricular systolic/diastolic volumes are currently used to determine PVR timing, but there are recognized limitations. Unique hemodynamic features in the pulmonary arteries of these patients have been found using 4D flow cardiovascular magnetic resonance (CMR), which we hypothesize may inform PVR timing.
Hypothesis
Hemodynamic alterations in the pulmonary arteries of rTOF patients may inform timing of PVR.
Aims
To compare pulmonary arterial hemodynamics for rTOF patients who were/were not indicated for PVR after the exams using 4D flow CMR.
Methods
Clinical 4D flow CMR exams of rTOF patients were accessed retrospectively with IRB approval. Patients were classified into two groups depending on whether they underwent PVR after the CMR exam. Age-matched controls’ 4D flow data were also included. After pre-processing of 4D flow, the right ventricular outflow tract, main, left and right pulmonary arteries (RVOT, MPA, LPA and RPA) were manually segmented from phase-contrast magnetic resonance angiography. In addition to basic flow metrics such as regurgitant fraction, systolic and diastolic averages of helicity, vorticity, and viscous energy loss were computed for the four subdomains using an automated pipeline (Fig.1). Indexed end-systolic/diastolic right ventricular volumes were obtained from clinical CMR reports. P<0.05 was considered statistically significant.
Results
Eighteen controls (age, 14.9 [11.7-17.0] years) and 21 rTOF patients, consisting of 8 without PVR (noPVR; age, 14.7 [9.6-23.4] years) and 13 indicated for PVR after the exam (PVR; age, 16.1 [8.7 -20.3 years]; days between CMR and PVR, 134 [59.5 – 189.3] days), were included. The PVR group had significantly larger indexed right ventricular volume than the noPVR group (P=0.002; Table 1). Regurgitant fraction and diastolic vorticity at the LPA were significantly larger in the PVR group (P=0.007 for regurgitant fraction; P=0.02 for vorticity; Fig.2AB). Although not statistically significant, diastolic helicity at the MPA showed borderline significance (P=0.05; Fig.2C).
Conclusion
In addition to right ventricular dilatation and larger regurgitant fraction, patients indicated for PVR had larger vorticity in the LPA. This preliminary result could be used for future longitudinal study to determine hemodynamic markers that inform PVR timing. A larger cohort is under evaluation.
More abstracts on this topic:
A Case of Caseous Mitral Annular Calcification and the Utility of Multimodality Cardiac Imaging
Nguyen Amanda, English Carter, Ghasemiesfe Ahmadreza, Venugopal Sandhya
Cardiovascular magnetic resonance imaging estimation of diffuse myocardial and hepatic fibrosis late after tetralogy of Fallot repairMarques Lais, Rani Karur Gauri, Chaturvedi Rajiv, Friedberg Mark, Epelman Slava, Roche Susan, Wald Rachel, Ishikita Ayako, Kuruvilla Thomas Subin, Begun Isaac, Dsouza Romina, Du Plessis Jacques, Asakawa Soshun, Yuen Daren, Hanneman Kate