Final ID: Mo3082
How many and which leads in ECG do you need to estimate a patient’s ejection fraction? A Deep Learning Approach.
Abstract Body (Do not enter title and authors here): Patients with heart failure (HF) can range from being asymptomatic to experiencing various combinations of symptoms. Left ventricular ejection fraction (EF), measured via echocardiography, is the primary tool to differentiate between different HF types and guide therapies. However, the availability of echocardiography varies geographically. In contrast, electrocardiograms (ECGs) are more common and easily accessible. In this study, we use a deep learning approach to correlate ECG readings with their corresponding EF. Low EF is defined as ≤ 35%.
Patients with the International Classification of Diseases codes for HF were screened retrospectively at Changhua Christian Hospital, Taiwan, from 2016 to 2022 with IRB approval. Only data comprising sex, age, a 10-second ECG record with a sampling rate of 500 Hz, and an echocardiography report obtained within 7 days after ECG acquisition were included. There were 3,508 samples (low EF: normal EF = 1,430:2,078) from 1,240 patients in the dataset. We reserved 10% of the samples as the final testing set (n=351) and split the remaining 90% randomly into the training and validation sets (n=2,525 and n=632) in a ratio of 8:2. A convolutional neural network was trained to classify input ECG lead(s) as either low or normal EF. For simplicity, the model with the lowest validation loss was selected and further evaluated on the final testing set.
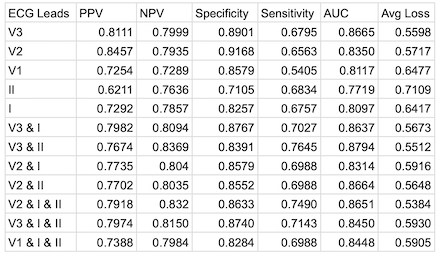
There were 721 males and 519 females with a mean age of 70.47 (±14.59). We experimented with various combinations of limb and chest leads as input ECG data and used the validation set to assess their performance, as shown in Table 1. The model trained with leads V2, I, and II had the lowest validation loss and achieved 71.3% sensitivity, 88.6% specificity, and an AUC of 87.6% on the testing set.
With more information from multiple leads, a patient’s EF could be better predicted; however, the incremental benefits tapered off quickly. In our investigation, the best model was found by combining information from three leads: I, II, and V2. Our study discovered a pathway to ECG-based artificial intelligence applications and provided innovative insights into medical device design, which could benefit patients in under-resourced areas.
Patients with the International Classification of Diseases codes for HF were screened retrospectively at Changhua Christian Hospital, Taiwan, from 2016 to 2022 with IRB approval. Only data comprising sex, age, a 10-second ECG record with a sampling rate of 500 Hz, and an echocardiography report obtained within 7 days after ECG acquisition were included. There were 3,508 samples (low EF: normal EF = 1,430:2,078) from 1,240 patients in the dataset. We reserved 10% of the samples as the final testing set (n=351) and split the remaining 90% randomly into the training and validation sets (n=2,525 and n=632) in a ratio of 8:2. A convolutional neural network was trained to classify input ECG lead(s) as either low or normal EF. For simplicity, the model with the lowest validation loss was selected and further evaluated on the final testing set.
There were 721 males and 519 females with a mean age of 70.47 (±14.59). We experimented with various combinations of limb and chest leads as input ECG data and used the validation set to assess their performance, as shown in Table 1. The model trained with leads V2, I, and II had the lowest validation loss and achieved 71.3% sensitivity, 88.6% specificity, and an AUC of 87.6% on the testing set.
With more information from multiple leads, a patient’s EF could be better predicted; however, the incremental benefits tapered off quickly. In our investigation, the best model was found by combining information from three leads: I, II, and V2. Our study discovered a pathway to ECG-based artificial intelligence applications and provided innovative insights into medical device design, which could benefit patients in under-resourced areas.
More abstracts on this topic:
A Case Presentation of Severe Left Ventricular Dysfunction from Focal Myocarditis due to Immune Checkpoint Inhibitor
Patel Romil, Hussain Kifah, Gordon Robert
A Simple One-Item Nursing Falls Assessment Predicts Outcomes For Patients With Stage D Heart Failure Undergoing Surgical Advanced TherapiesSalvador Vincent, Perez Jaime Abraham, Hudec Paige, Gorodeski Eiran, Oneill Thomas