Final ID: Sa4035
Impact of Stress Hyperglycemia Ratio on Heart Failure and Atherosclerotic Cardiovascular Events After Acute Myocardial Infarction
Abstract Body (Do not enter title and authors here): Background: An acute hyperglycemic status is reportedly associated with poor prognosis in patients with acute cardiovascular diseases. Although the stress hyperglycemia ratio (SHR) is a novel index to accurately represent the hyperglycemic condition on admission, relations between SHR and clinical outcomes are not fully evaluated in a setting of acute myocardial infarction (MI).
Methods: This retrospective, multicenter registry study included 2,386 patients with acute MI undergoing percutaneous coronary intervention. SHR was calculated as a blood glucose level on admission divided by the estimated average glucose derived from a glycated hemoglobin level. The co-primary endpoints of this study included heart failure (HF)-related events (a composite of all-cause death and worsening and hospitalized HF) and major atherosclerotic cardiovascular events (MACE) (a composite of all-cause death, recurrent MI, and ischemic stroke), during the index hospitalization and after discharge.
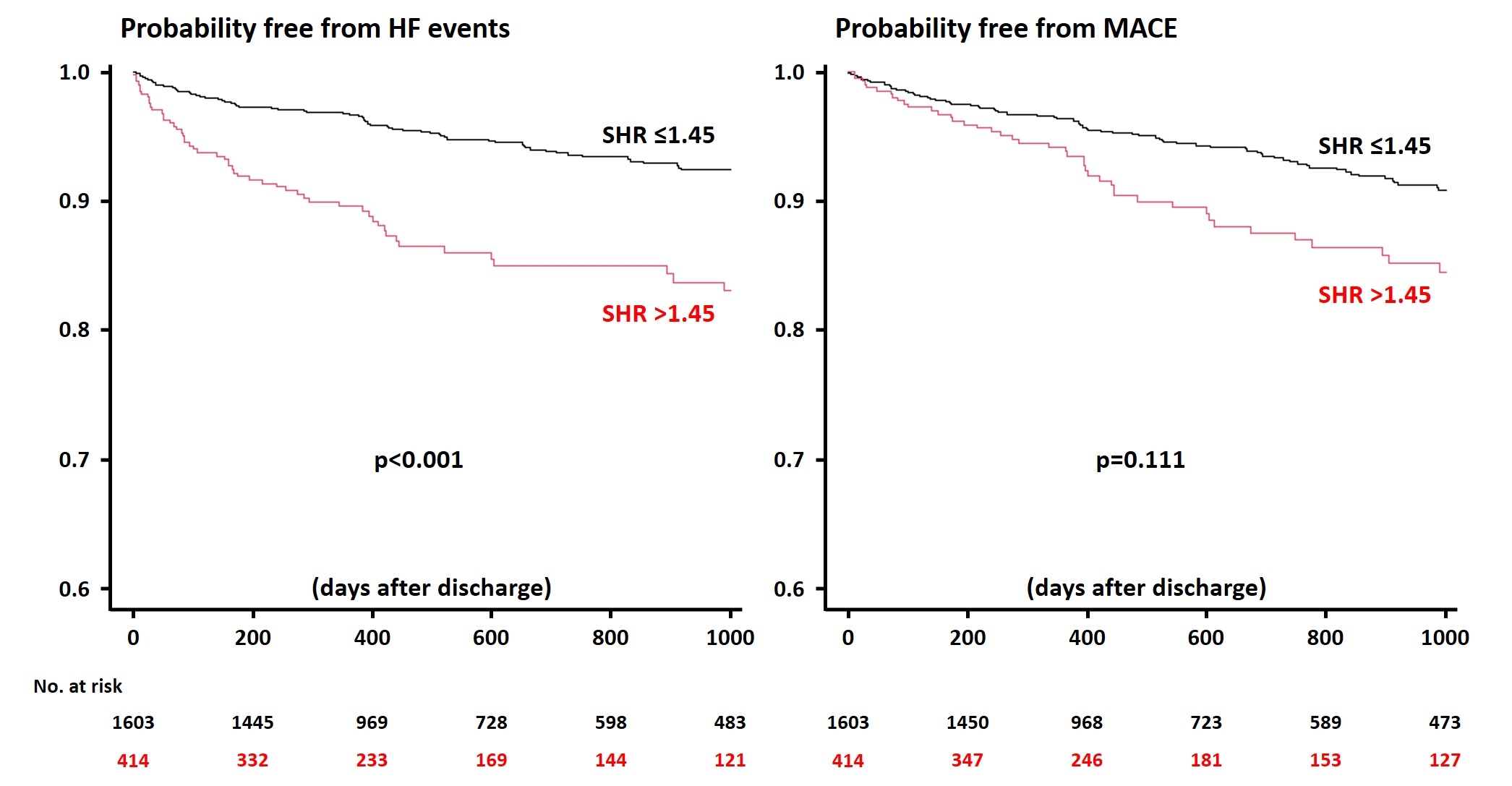
Results: Of the 2,386 patients, 890 (37.3%) had diabetes, and the median SHR was 1.17 [0.99, 1.45]. HF events and MACE occurred in 680 (28.5%) and 233 (9.8%) during hospitalization. SHR was identified as a factor significantly associated with both in-hospital HF events (adjusted odds ratio 1.65, 95% confidence interval 1.18-2.29, p=0.003) and MACE (adjusted odds ratio 1.50, 95% confidence interval 1.10-2.03, p=0.009). Among 2,017 patients who survived to discharge and had follow-up information, 195 (9.7%) and 214 (10.6%) experienced HF events and MACE during the median of 536 days after discharge. Patients with the high SHR (>1.45, 4th quartile) had an increased risk of HF events than those with SHR ≤1.45, while the incidence of MACE after discharge did not differ significantly between the two groups (Figure). The multivariable analysis confirmed the association of SHR with long-term HF events.
Conclusions: In patients with acute MI, SHR was predictive of in-hospital outcomes including HF events and MACE, while after discharge, the higher SHR was associated with a higher HF risk but not with MACE. Further studies are needed to elucidate the underlying mechanisms and potential incremental benefit of SHR in stratifying patient risks after MI.
Methods: This retrospective, multicenter registry study included 2,386 patients with acute MI undergoing percutaneous coronary intervention. SHR was calculated as a blood glucose level on admission divided by the estimated average glucose derived from a glycated hemoglobin level. The co-primary endpoints of this study included heart failure (HF)-related events (a composite of all-cause death and worsening and hospitalized HF) and major atherosclerotic cardiovascular events (MACE) (a composite of all-cause death, recurrent MI, and ischemic stroke), during the index hospitalization and after discharge.
Results: Of the 2,386 patients, 890 (37.3%) had diabetes, and the median SHR was 1.17 [0.99, 1.45]. HF events and MACE occurred in 680 (28.5%) and 233 (9.8%) during hospitalization. SHR was identified as a factor significantly associated with both in-hospital HF events (adjusted odds ratio 1.65, 95% confidence interval 1.18-2.29, p=0.003) and MACE (adjusted odds ratio 1.50, 95% confidence interval 1.10-2.03, p=0.009). Among 2,017 patients who survived to discharge and had follow-up information, 195 (9.7%) and 214 (10.6%) experienced HF events and MACE during the median of 536 days after discharge. Patients with the high SHR (>1.45, 4th quartile) had an increased risk of HF events than those with SHR ≤1.45, while the incidence of MACE after discharge did not differ significantly between the two groups (Figure). The multivariable analysis confirmed the association of SHR with long-term HF events.
Conclusions: In patients with acute MI, SHR was predictive of in-hospital outcomes including HF events and MACE, while after discharge, the higher SHR was associated with a higher HF risk but not with MACE. Further studies are needed to elucidate the underlying mechanisms and potential incremental benefit of SHR in stratifying patient risks after MI.
More abstracts on this topic:
ACLY Inhibition as a Novel Therapeutic Approach for Vascular Remodeling in Coronary Artery Disease.
Grobs Yann, Reem El-kabbout, Potus Francois, Provencher Steeve, Boucherat Olivier, Bonnet Sebastien, Romanet Charlotte, Lemay Sarah-eve, Bourgeois Alice, Voisine Pierre, Theberge Charlie, Sauvaget Melanie, Breuils Bonnet Sandra, Martineau Sandra
Early GLP-1 Receptor Agonist Initiation Reduces Major Cardiac and Renal Events in Older Adults with Type 2 Diabetes Without Prior Cardiovascular or Renal Disease: A Target Trial EmulationChi Kuan Yu, Chang Yu, Varrias Dimitrios, Nanna Michael, Nouri Armin, Lee Pei-lun, Hsieh Rebecca, Mangalesh Sridhar, Hu Jiun-ruey, Ezenna Chidubem, Akman Zafer, Romero Acero Laura