Final ID: Sa2136
Abatacept Drug-Induced Loeffler Endocarditis: A Manifestation of Hypereosinophilic Syndrome
Abstract Body (Do not enter title and authors here): Description of Case:
This case presents a 32-year-old woman with history of rheumatoid arthritis who presented with symptoms of worsening dyspnea on exertion, fatigue, and stable angina five weeks after starting abatacept.
Methods:
Performed a comprehensive retrospective analysis of one patient's medical history, clinical presentation, diagnostic assessment, therapeutic intervention, and clinical outcome.
Results:
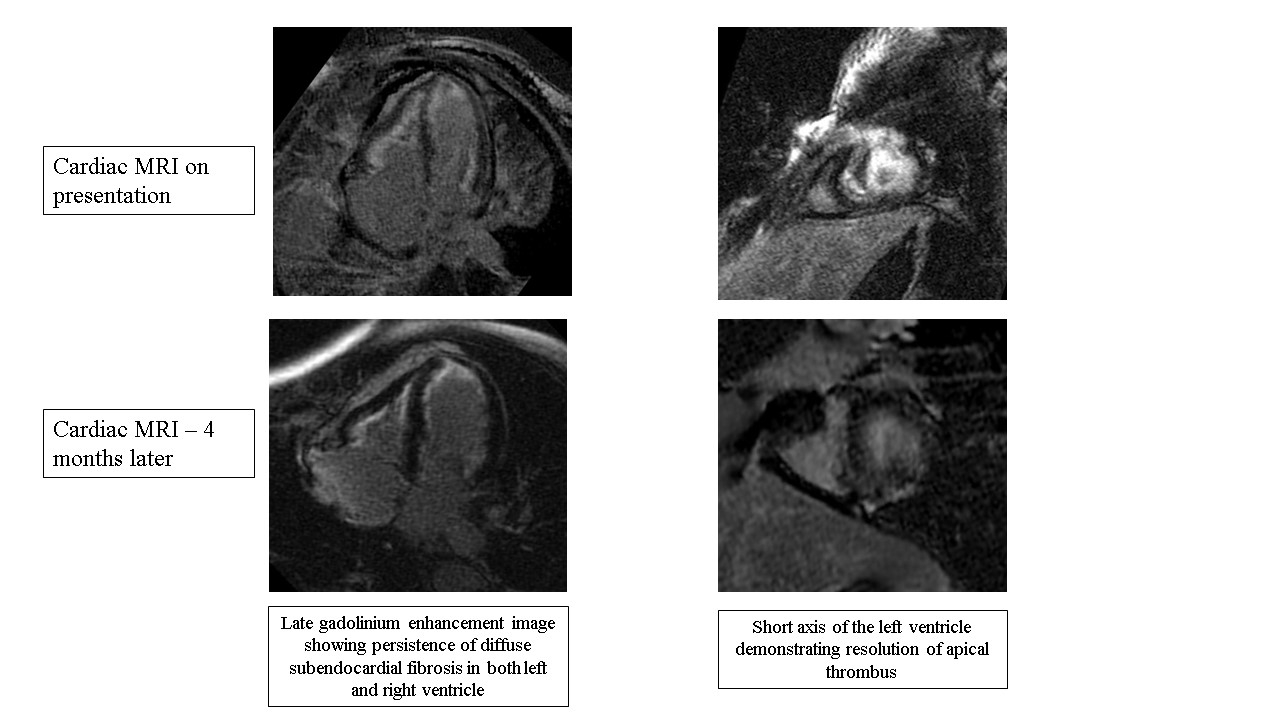
Physical exam was remarkable for signs of volume overload. Electrocardiogram showed sinus tachycardia and diffuse nonspecific T-wave inversions. Laboratory studies revealed a complete blood count significant for eosinophilia of 26,000, representing 79.5% of the differential. Troponins were negative. A brain natriuretic peptide was 903 pg/ml. Echocardiogram findings included mild reduction in biventricular systolic function with wall motion abnormality seen at the apex. Cardiac MRI (CMR) demonstrated mild biventricular systolic dysfunction, left ventricular intracavitary filling defect consistent with thrombi, and diffuse biventricular subendocardial late gadolinium enhancement (LGE) consistent with fibrosis. Abatacept was stopped with resolution of eosinophilia. Patient was treated with a short course of steroids and initiated on warfarin for left ventricular thrombi. Repeat CMR four months later showed resolution of left ventricular thrombi and biventricular dysfunction, with persistence of diffuse subendocardial fibrosis in both left and right ventricles.
Discussion:
CMR demonstrates findings consistent with Loeffler Endocarditis as evident by ventricular intracavitary filling defects and diffuse biventricular subendocardial late gadolinium enhancement. Initial management of involves prompt discontinuation of the suspected offending drug. Corticosteroids may be employed to mitigate eosinophilic infiltrate and myocardial inflammation. Diagnostic modalities such as cardiac imaging, endomyocardial biopsy, and laboratory testing play crucial roles in confirming the diagnosis and assessing severity. Follow-up CMR can help follow the response to cessation of the offending agent and rule-out confounding disease processes, as seen in this case. In conclusion, abatacept-induced eosinophilic endocarditis is a rare phenomenon that is poorly understood. Drug-induced eosinophilic endocarditis should be considered as a differential in patients that develop heart failure symptoms and eosinophilia after initiating abatacept.
This case presents a 32-year-old woman with history of rheumatoid arthritis who presented with symptoms of worsening dyspnea on exertion, fatigue, and stable angina five weeks after starting abatacept.
Methods:
Performed a comprehensive retrospective analysis of one patient's medical history, clinical presentation, diagnostic assessment, therapeutic intervention, and clinical outcome.
Results:
Physical exam was remarkable for signs of volume overload. Electrocardiogram showed sinus tachycardia and diffuse nonspecific T-wave inversions. Laboratory studies revealed a complete blood count significant for eosinophilia of 26,000, representing 79.5% of the differential. Troponins were negative. A brain natriuretic peptide was 903 pg/ml. Echocardiogram findings included mild reduction in biventricular systolic function with wall motion abnormality seen at the apex. Cardiac MRI (CMR) demonstrated mild biventricular systolic dysfunction, left ventricular intracavitary filling defect consistent with thrombi, and diffuse biventricular subendocardial late gadolinium enhancement (LGE) consistent with fibrosis. Abatacept was stopped with resolution of eosinophilia. Patient was treated with a short course of steroids and initiated on warfarin for left ventricular thrombi. Repeat CMR four months later showed resolution of left ventricular thrombi and biventricular dysfunction, with persistence of diffuse subendocardial fibrosis in both left and right ventricles.
Discussion:
CMR demonstrates findings consistent with Loeffler Endocarditis as evident by ventricular intracavitary filling defects and diffuse biventricular subendocardial late gadolinium enhancement. Initial management of involves prompt discontinuation of the suspected offending drug. Corticosteroids may be employed to mitigate eosinophilic infiltrate and myocardial inflammation. Diagnostic modalities such as cardiac imaging, endomyocardial biopsy, and laboratory testing play crucial roles in confirming the diagnosis and assessing severity. Follow-up CMR can help follow the response to cessation of the offending agent and rule-out confounding disease processes, as seen in this case. In conclusion, abatacept-induced eosinophilic endocarditis is a rare phenomenon that is poorly understood. Drug-induced eosinophilic endocarditis should be considered as a differential in patients that develop heart failure symptoms and eosinophilia after initiating abatacept.
More abstracts on this topic:
A Predictive Tool and Diagnostic Screening Algorithm for the Identification of Transthyretin Amyloid Cardiomyopathy in High-Risk Patient Populations
Chai Jocelyn, Sathananthan Janarthanan, Fine Nowell, Davis Margot, Starovoytov Andrew, Campbell Christine, Hawkins Nathaniel, Virani Sean, Luong Michael, Straatman Lynn, Kiess Marla, Worsley Daniel
A REPORT OF >2000 CONSECUTIVE NON-SELECTED PATIENTS UNDERGOING IMAGING WITH PACEMAKER'S AND ICD'S IN THE MRI ENVIRONMENT; THE ADDITIVE VALUE OF A LARGE, PROSPECTIVE >20-YEAR OBSERVATIONAL STUDYBiederman Robert, Shah Moneal, Lombardi Rich, Boltralik Mark, Mangini Francesco, Doyle Mark